The National Association of Nurse Practitioners in Women’s Health (NPWH) affirms that women’s health nurse practitioners (WHNPs) and other advanced practice registered nurses (APRNs) who provide healthcare for women across the lifespan have a critical role in cardiovascular disease (CVD) risk screening and implementation of primary prevention strategies to improve the cardiovascular health of women. NPWH promotes a person-centered cardiovascular health approach based on currently recognized guidelines, appropriate use of risk assessment tools, attention to social determinants of health (SDOH), and shared decision making about best strategies to reduce CVD risk. A multidisciplinary health professional team-based approach has the potential to improve outcomes for ongoing CVD prevention, especially when an individual is determined to be at higher risk because of comorbidities or family history of premature CVD. NPWH asserts that SDOH-mediated inequities in cardiovascular care and outcomes must be addressed at all levels through changes in healthcare systems, health professional education, public health measures, and culturally competent team-based healthcare delivery.
Public awareness of CVD as the leading cause of death among women declined from 2009 (65%) to 2019 (44%).1 The decline in awareness was most prominent among women age 25 to 34 years, Hispanic and non-Hispanic Black women, and individuals with lower educational attainment.1 NPWH supports an escalation of efforts to inform the public about CVD among women through awareness campaigns. These campaigns should be culturally and linguistically appropriate and provided through venues that will reach those most in need of increased awareness.
Women, gender-diverse individuals, and all socioeconomic, ethnic, and racial populations must be fully represented in research on which guidelines for prevention of CVD are based. Current knowledge should be widely disseminated and used in quality improvement initiatives to implement CVD prevention guidelines and evaluate outcomes at clinical and healthcare system levels. NPWH emphasizes that the women’s health expertise of WHNPs makes them critical partners and leaders in these research and quality improvement endeavors.
Background
Cardiovascular disease is the leading cause of morbidity and mortality for women in the United States and worldwide. In fact, more than 1 in 4 women (27.2%) in the US die from CVD.2
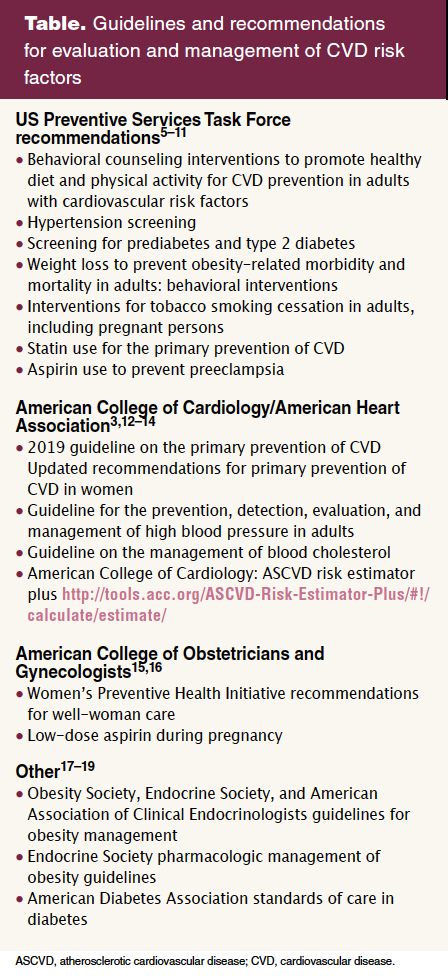
While prevalence increases with age, it is significant that 11% of women have some form of CVD before they reach the age of 60 years.2 Traditional risk factors for CVD are well established and include family history, smoking, physical inactivity, unhealthy diet, hypertension, hyperlipidemia, diabetes, and obesity.3,4 Guidelines and recommendations are available to address evaluation and behavioral and pharmacologic management of several of these risk factors (Table).3,5–19
Social determinants of health influence cardiovascular health, CVD risks, and CVD outcomes.3,20–22 Structural racism and discrimination, rejection, and victimization of individuals that have been marginalized because of racial, ethnic, sexual orientation, gender identity or other status are recognized as key drivers in SDOH adversities that result in inequities in healthcare and disparities in cardiovascular health.21 As well, adverse childhood experiences (eg, abuse, neglect, household dysfunction) and stress-related mental health conditions such as depression and posttraumatic stress disorder are associated with an increased long-term risk of CVD.23,24 Attention to SDOH, psychosocial stressors, and mental health are important components for reducing CVD risk and enhancing cardiovascular health.
An accurate estimate of CVD risk provides the starting point for risk reduction discussions.3,25 Quantitative risk assessment tools to estimate 10-year CVD risk for individuals age 40 to 75 years or lifetime risk for individuals age 20 to 39 years are available online, as mobile applications, and within some electronic health record platforms.25 It is important to keep in mind that these risk assessment tools are population based and can under- or overestimate an individual’s risk. Shared decision making about risk reduction can be individualized based on risk estimate, personal preferences, and the presence of other CVD risks not included in the assessment tool.
Although more research is needed, studies are now elucidating critical evidence about CVD risk enhancers that are unique to biologic females. Risk enhancers extend to pregnancy-associated conditions and other health conditions with associated sex-hormone factors. These conditions are not currently included in available quantitative risk assessment tools. Studies are being conducted to determine if their inclusion would add benefit in predicting CVD risk in women.22,26 The 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease and 2018 Guideline on the Management of Blood Cholesterol include a history of pregnancy-associated conditions that increase CVD risk such as preeclampsia and a history of premature menopause (before age 40) as risk enhancers.3,14 The association between these conditions and increased risk for future CVD is hypothesized to be related to vascular endothelial dysfunction, an early marker of atherosclerosis.4,27,28 Further research is needed to understand how these conditions contribute to inflammatory changes with long-term effects on vascular endothelium and if there may be bi-directional associations.4,27,28
All hypertensive disorders of pregnancy are associated with an increased risk of chronic hypertension as early as the first year after giving birth. A large meta-analysis found that after 10 to 15 years, individuals who had experienced preeclampsia had a 3.7-fold risk of hypertension, 2.2-fold risk of ischemic heart disease, and 1.8-fold risk of stroke.29 Individuals with a history of gestational diabetes also are at an increased risk of future CVD. They have an up to 20-fold risk of type 2 diabetes, 2-fold increased risk of hypertension, 2.8-fold risk of ischemic heart disease, and 2-fold increased risk of stroke.30 Other adverse pregnancy outcomes (APOs) that have been associated with an increased risk of CVD include preterm birth, pregnancy loss, intrauterine growth restriction, and placental abruption.12,21
Strategies for mitigating future CVD include identifying individuals who have experienced these associated APOs, encouraging lactation beyond 6 months for its cardioprotective effects, screening for other risk factors, lifestyle behavior counseling, ongoing monitoring, and implementing interventions to reduce risks for APOs in subsequent pregnancies.26,31,32 Growing evidence supports associations between cardiovascular health prior to pregnancy and APOs. As well, CVD is the major causative condition related to perinatal morbidity and mortality in the US.33 Guidelines and recommendations in the Table can be incorporated into wellness, prepregnancy care, and interpregnancy care to promote cardiovascular health.
Hormonal factors identified as risk enhancers for CVD include those which occur with polycystic ovary syndrome (PCOS), primary ovarian insufficiency (POI), and premature menopause. PCOS is the most common endocrine disorder among women of reproductive age, affecting 5% to 13% of the population.34 PCOS, particularly the hyperandrogenic phenotypes, is associated with several cardiometabolic comorbidities including obesity, dyslipidemia, elevated blood pressure, and prediabetes or type 2 diabetes.34,35 Some studies have suggested that PCOS is associated with increased risk for CVD independent of traditional risk factors.36 Although further study is needed to determine causality, individuals with PCOS benefit from CVD risk screening with lifestyle management and pharmacotherapy to improve their metabolic profile and reduce CVD risk. Recommendations from international evidence-based guidelines specifically address CVD risk assessment components for individuals with PCOS.37
Premature menopause (natural, surgical, or treatment-induced) is defined as permanent cessation of menses before age 40 years, and early menopause is defined as occurring between the ages of 40 and 45 years. POI describes the loss of ovarian function before age 40 but with the potential for intermittent, transient return of hormone production and menstrual cycles.38 These conditions result in prolonged postmenopausal estrogen levels or estrogen deficiency in younger women and have been demonstrated to increase the risk for CVD.39,40 Further research is needed to understand the mechanisms for the association of premature estrogen deficiency and CVD risk.39,40 Assessment of overall CVD risk should include recognition of this risk enhancer. Individuals experiencing premature menopause or POI benefit from education concerning their CVD risk, lifestyle modifications to reduce this risk, potential consideration of preventive use of statins related to adjusted risk level, and use of estrogen replacement therapy.14,37 Estrogen replacement therapy is approved by the US Food and Drug Administration (FDA) for women with premature hypoestrogenism resulting from hypogonadism, bilateral oophorectomy (BO), or POI.31 Beyond the recognized health benefit of prevention of bone loss, observational studies have shown evidence of benefit in reducing the risk for heart disease, most especially for individuals with BO.37 It is recommended that estrogen be continued at least until the average age of menopause, which is approximately 52 years.37,40
The menopause transition when it occurs normally in midlife represents a period of accelerated CVD risk. Changes in body mass index and fat distribution; acceleration of total and low-density-lipoprotein cholesterol levels; increase in systolic blood pressure; and a noted decrease in consistent physical activity and healthy diet all may increase CVD risk during the menopause transition.41 CVD risk assessment in this age group, counseling for heart-healthy lifestyles, and strategies to mitigate specifically identified risks are essential. Hormone therapy is not FDA approved for the prevention of CVD in women experiencing normally timed menopause. It is FDA approved for the management of moderate-to- severe menopause-related vasomotor and vulvovaginal symptoms and to prevent postmenopausal osteoporosis. The North American Menopause Society 2022 hormone therapy position statement is a resource for guidance.37
Data from studies on hormone therapy and CVD risk for cisgender women cannot be extrapolated to gender-affirming hormone therapy for transgender women. One large study showed an increased risk for venous thromboembolism, myocardial infarction, and ischemic stroke in transgender women taking estrogen compared with cisgender men not taking any hormones.42 More study is needed in this area. Assessment for other CVD risks, discussion of individual risks and benefits, and ongoing monitoring should inform shared decision making.
Implications for practice
Women’s health nurse practitioners and other APRNs who provide women’s and gender-related healthcare have opportunities in any clinical setting to promote cardiovascular health, identify CVD risk factors, evaluate for and attend to SDOH adversely affecting cardiovascular care and outcomes, and use person-centered, shared decision making to choose strategies to reduce risk. They have an important leadership role in development, implementation, and outcome evaluation of initiatives for the use of evidence-based guidelines at the clinical and organizational level. Their collaboration with other primary care providers, nutritionists, mental and behavioral health professionals, and cardiology specialists allows for a team-based approach to meet individual needs and enhance cardiovascular health outcomes.
NPWH leadership
NPWH will provide leadership to ensure:
- Continuing education programs and resources are available to support WHNPs and other APRNs who provide women’s and gender-related healthcare in person-centered CVD risk assessment and risk reduction.
- WHNP educational programs have access to evidence-based information on person-centered CVD risk assessment and risk reduction in women’s and gender-related healthcare that can be incorporated into curricula.
- Collaborative engagement with other organizations that supports campaigns to increase public awareness about CVD risk and CVD prevention in women.
- Advocacy for health policies that address SDOH influencing cardiovascular health.
- Research progresses to identify effective CVD risk screening and risk reduction strategies for women and gender-diverse individuals.
References
1 Cushman M, Shay CM, Howard VJ, et al; American Heart Association. Ten-year differences in women’s awareness related to coronary heart disease: results of the 2019 American Heart Association national survey: a special report from the American Heart Association. Circulation. 2021;143(7):e239–e248.
2 Tsao CW, Aday AW, Almarzoog ZI, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation. 2023;147(8):e93-e621.
3 Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e563–e595.
4 Liu E, Bigeh A, Ledingham L, Mehta L. Prevention of coronary artery disease in women. Curr Cardiol Rep. 2022;24(8):1041-1048.
5 US Preventive Services Task Force; Krist AH, Davidson KW, Mangione CM, et al. Behavioral counseling interventions to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US Preventive Services Task Force recommendation statement. JAMA. 2020;324(20):2069-2075.
6 US Preventive Services Task Force; Krist AH, Davidson KW, Mangione CM, et al. Screening for hypertension in adults: US Preventive Services Task Force reaffirmation recommendation statement. JAMA. 2021;325(16):1650-1656.
7 US Preventive Services Task Force; Davidson KW, Barry MJ, Mangione CM, et al. Screening for prediabetes and type 2 diabetes: US Preventive Services Task Force recommendation statement. JAMA. 2021;326(8):736-743.
8 US Preventive Services Task Force; Curry SJ, Krist AH, Owens DK, et al. Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: US Preventive Services Task Force recommendation statement. JAMA. 2018;320(11):1163-1171.
9 US Preventive Services Task Force; Krist AH, Davidson KW, Mangione CM, et al. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force recommendation statement. JAMA. 2021;325(3):265-279.
10 US Preventive Services Task Force; Mangione CM, Barry MJ, Nicholson WK, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2022;322(8):746-753.
11 US Preventive Services Task Force; Davidson KW, Barry MJ, Mangione CM, et al. Aspirin use to prevent preeclampsia and related morbidity and mortality: US Preventive Services Task Force recommendation statement. JAMA. 2021;326(12):1186-1191.
12 Cho L, Davis M, Elgendy I, et al; ACC CVD Womens Committee Members. Summary of updated recommendations for primary prevention of cardiovascular disease in women: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(20):2602-2618.
13 Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/ AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248.
14 Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/ American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;139(25):e1082-e1143.
15 Women’s Preventive Services Initiative. Well-Woman Chart. Recommendations for Well-Woman Care. 2022. https://www.womenspreventivehealth.org/wellwomanchart
16 American College of Obstetricians and Gynecologists. ACOG Committee Opinion no. 743. Low-dose aspirin use during pregnancy. Obstet Gynecol. 2018;132(1):e44-e52.
17 Ryan DH, Kahan S. Guideline recommendations for obesity management. Med Clin North Am. 2018;102(1):49-63.
18 Apovian CM, Aronne LJ, Bessesen DH, et al; Endocrine Society. Pharmacological management of obesity: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(2):342-362.
19 ElSayed NA, Aleppo G, Aroda VR, et al. Improving care and promoting health in populations: standards of care in diabete–2023. Diabetes Care. 2023;46(suppl 1):S10-S18.
20 Javed Z, Haisum Maqsood M, Yahya T, et al. Race, racism, and cardiovascular health: applying a social determinants of health framework to racial/ethnic disparities in cardiovascular disease. Circ Cardiovasc Qual Outcomes. 2022;15(1):72-86.
21 Mannoh I, Hussien M, Commodore-Mensah Y, Michos ED. Impact of social determinants of health on cardiovascular disease prevention. Curr Opin Cardiol. 2021;36(5):572-579.
22 Wenger NK, Lloyd-Jones DM, Elkind MSV, et al. Call to action for cardiovascular disease in women: epidemiology, awareness, access, and delivery of equitable health care: a presidential advisory from the American Heart Association. Circulation. 2022;145(23):e1059-e1071.
23 Vaccarino V, Bremmer JD. Behavioral, emotional and neurobiological determinants of coronary heart disease risk in women. Neurosci Biobehav Rev. 2017;74(Pt B):297-309.
24 Godoy LC, Frankfurter C, Cooper M, et al. Association of adverse childhood experiences with cardiovascular disease later in life: a review. JAMA Cardiol. 2021;6(2):228-235.
25 Lloyd-Jones DM, Braun LT, Ndumele CE, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2019;73(24):3153–3167.
26 Park K, Minissian MB, Wei J, et al. Contemporary clinical updates on the prevention of future cardiovascular disease in women who experience adverse pregnancy outcomes. Clin Cardiol. 2020;43(6):553-559.
27 Elder P, Sharma G, Gulati M, Michos ED. Identification of female-specific risk enhancers throughout the lifespan of women to improve cardiovascular disease prevention. Am J Prev Cardiol. 2020;2:100028.
28 O’Kelly AC, Michos ED, Shufelt CL, et al. Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ Res. 2022;130(4):652-672.
29 Bellamy L, Casas J-P, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974.
30 Daly B, Toulis KA, Thomas N, et al. Increased risk of ischemic heart disease, hypertension, and type 2 diabetes in women with previous gestational diabetes mellitus, a target group in general practice for preventive interventions: a population-based cohort study. PLoS Med. 2018;15(1):e1002488.
31 Bottone-Post CL. Development of cardiovascular disease after adverse pregnancy outcome. Womens Healthcare. 2022;10(6):19-24.
32 Parikh NI, Gonzalez JM, Anderson CAM, et al; American Heart Association Council on Epidemiology and Prevention; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; and the Stroke Council. Adverse pregnancy outcomes and cardiovascular disease risk: unique opportunities for cardiovascular disease prevention in women: a scientific statement from the American Heart Association. Circulation. 2021;143(18):e902-e916.
33 Khan SS, Brewer LC, Canobbio MM, et al; American Heart Association Council on Epidemiology and Prevention; Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Hypertension; Council on Lifestyle and Cardiometabolic Health; Council on Peripheral Vascular Disease; and Stroke Council. Optimizing prepregnancy cardiovascular health to improve outcomes in pregnant and postpartum individuals and offspring: a scientific statement from the American Heart Association. Circulation. 2023;147(7):e76-e91.
34 Guan C, Zahid S, Minhas AS, et al. Polycystic ovary syndrome: a “risk-enhancing” factor for cardiovascular disease. Fertil Steril. 2022;117(5):924-935.
35 Rollene NL, Lentscher JA, Hemphill AM, Decherney AH. Polycystic ovary syndrome and medical conditions. Clin Obstet Gynecol. 2020;64(1):110-118.
36 Teede HJ, Misso ML, Costello MF, et al; International PCOS Network. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018;110(3):364-379.
37 North American Menopause Society Advisory Panel. The 2022 hormone therapy position statement of the North American Menopause Society. Menopause. 2022;29(7):767-794.
38 Honigberg MC, Zekavat SM, Aragam K, et al. Association of premature natural and surgical menopause with incident cardiovascular disease. JAMA. 2019;322(24):2411-2421.
39 Price MA, Alvarado BE, Rosendaal NTA, et al. Early and surgical menopause associated with higher Framingham risk scores for cardiovascular disease in the Canadian Longitudinal Study on Aging. Menopause. 2021;28(5):484-490.
40 Sullivan SD, Sarrel PM, Nelson LM. Hormone replacement therapy in young women with primary ovarian insufficiency and early menopause. Fertil Steril. 2016;106(7):1588-1599.
41 El Khoudary SR, Aggarwal B, Beckie TM, et al; American Heart Association Prevention Science Committee of the Council on Epidemiology and Prevention; and Council on Cardiovascular and Stroke Nursing. Menopause transition and cardiovascular disease risk: implications for timing of early prevention: a scientific statement from the American Heart Association. Circulation. 2020;142(25):e506-e532.
42 Getahun D, Nash R, Faldners WD, et al. Cross-sex hormones and acute cardiovascular events in transgender persons: a cohort study. Ann Intern Med. 2018;169(4):205-213.
NPWH gratefully acknowledges Carolyn Bottone-Post, DNP, CNM; Lynne Braun, PhD, CNP; Beth Kelsey, EdD, APRN, WHNP-BC; Jean Marino, APRN, WHNP-BC; and Ludrena Rodriguez, DNP, WHNP-BC, for their contributions as writing group members of this position statement.
Approved by the NPWH Board of Directors: April 13, 2023