Collection of a patient’s family history (FH) is an important tool for establishing her risk levels for certain inherited cancers. Time constraints and other barriers challenge the ability of healthcare providers to collect a complete and detailed FH, which can result in inadequate risk assessment. The author presents strategies to improve FH collection and documentation and briefly reviews guidelines for assessing patterns of risk for inherited cancers within the history.
Key words: family history, inherited cancer, genetic testing, breast cancer
In clinical practice, a patient’s family history (FH) helps establish patterns of risk for hereditary disease and serves as a component of the general health history. Collection of an FH that reflects three or more generations (siblings, parents, grandparents) is recommended to assess a patient’s genetic risk for hereditary cancers. In many cases, FHs are limited to information about first-degree relatives; these histories are rarely updated to reflect newly discovered disease in family members.1 Lack of availability or inadequate review of the FH is a missed opportunity for risk stratification for hereditary cancers, referral for genetic testing, and provision of recommendations for early screening and risk reduction strategies if needed.
Healthcare providers (HCPs) should take a complete FH at each patient’s annual well-woman visit and be able to recognize patterns of risk for inherited cancers. A woman’s genetic predisposition to hereditary cancer will have implications for screening, disease prevention, and treatment options.2 The purpose of this article is to improve the quality of FH documentation by presenting strategies to streamline collection of FH information and to review guidelines for assessing patterns of risk for inherited cancers—specifically breast cancer, reproductive cancers, and colon cancer—within the history.
Inherited genetic mutations that increase cancer risk
Although generally recognized as a risk factor for breast cancer, a mutation of breast cancer gene 1 or 2 (BRCA 1/2) imparts substantial risk for the development of other cancers as well. A mutation in BRCA 1/2 disables the ability of the gene to affect cellular repair of damaged DNA, a condition particularly associated with breast, ovarian, prostate, and pancreatic cancers.3 The pattern of inheritance is autosomal-dominant; inheritance of the BRCA 1/2 mutation may arise from either the maternal or the paternal side of the family. Women who carry a mutation on BRCA 1/2 have a 40%-80% risk of developing breast cancer and a 11%-40% risk of developing ovarian cancer in their lifetime.4 Mutations on other genes (TP53, PTEN, STK11) have been linked to high risk for breast cancer in young women, but these mutations are less common.5
Lynch syndrome (hereditary nonpolyposis colon cancer [HNPCC]), another autosomal-dominant genetic condition, places individuals at high risk for cancer by inactivating the DNA repair function coded by MSH2, a DNA mismatch repair protein, or by the gene MLH1.6 Women with Lynch syndrome have lifetime risks of 40%-60% of developing endometrial cancer and of 4%-12% of developing ovarian cancer.7,8 Women and men with this genetic condition have an 80% lifetime risk of developing colon cancer.9
Importance and implications of the family history review
For young women with no personal history of cancer (unaffected women), an FH review is an opportunity to provide anticipatory guidance. When an FH may indicate an inherited cancer, testing for the suspected genetic mutation in the affected family member(s) is recommended. Once a particular genetic mutation is identified in the family member(s), other members can be offered early screening and specific testing for the mutation.5 Early awareness is important; women who test positive for a genetic mutation that imparts cancer risk should be counseled about early screening and consideration of preventive options.
For example, emerging data have associated the BRCA1 mutation with the development of cancers caused by the deleterious effect of estrogen metabolites on DNA synthesis. This link is noteworthy in that medications that decrease or halt estrogen production (e.g., luteinizing hormone-releasing agonists) could be offered as a preventive option against breast cancer for some women.10 Studies evaluating the effectiveness of aromatase inhibitors and selective estrogen receptor modulators for cancer prevention in these groups are under way. New evidence suggests that women with BRCA1 mutations who undergo oophorectomy before age 35 have decreased mortality rates from ovarian cancer (women who have BRCA2 mutations may be able to delay this surgery until their 40s).11 Oral contraceptive use and oophorectomy are recommended for prevention of HNPCC-related cancers.8
Of note, mutations in cancer predisposition genes other than BRCA1/2 and those that cause HNPCC can place women at high risk of developing breast cancer and/or reproductive cancers. Women who test negative for BRCA or HPNCC mutations but have a strong familial picture for cancer risk should begin screening early, and options for preventive treatment should still be considered.12
Family history collection methods
Many HCPs recognize the value of the FH but cite lack of time and limited patient knowledge of their own FH as major barriers to collection of an accurate FH.13 Several studies have established that a self-collected instrument is an effective and time-efficient method of collecting FH data and identifying risk for hereditary cancers.1,14,15 Individuals who self-collect may have access to family members with better recall for third- or fourth-degree relatives.14,15 Although initiatives to develop and improve access to self-collected and archived FHs are under way, adoption of this method has been slow.16,17
The Table lists some available FH tools. The Surgeon General’s Family History Initiative advocates use of an online tool, My Family Health Portrait (MFHP), which allows individuals to collect and upload accurate FH information. The MFHP facilitates creation of a table that can be populated online and downloaded for storage and periodic updating on a computer. The printed output can be shared with HCPs to help identify specific risk patterns within the family.16,18 Although few studies have been published on the efficacy of MFHP, evidence suggests that this tool is particularly useful as a means of recording FHs of breast and ovarian cancers.19,20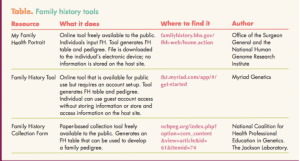
Family Healthware™, developed by the CDC, is a Web-based tool that integrates familial risk assessment with generation of specific health screening recommendation messages based on risk.21 Although the results of a randomized trial conducted on 3283 primary care patients that compared the clinical usefulness of the Family Healthware tool versus general cancer prevention messages were equivocal,21 the authors suggested that better engagement with the clinician and integration with a health record and decision support might improve clinical outcomes and should be incorporated in future iterations of the tool. As this issue goes to press, the CDC website for Family Healthware indicates that the Web-based tool remains in testing but may be available for research purposes by contacting the CDC.22
Myriad Genetics created the Hereditary Cancer Quiz, a four-item online assessment that purports to identify flags for hereditary breast and ovarian cancer (HBOC) and HNPCC risks.23 Individuals whose answers trigger risk flags are invited to complete a detailed online Family History Tool (FHT). The FHT is similar to the MFHP in that individuals who complete the FHT can identify patterns showing risk for hereditary cancers within their family.24 The table and pedigree generated by the FHT can be shared with a specified HCP via encrypted email. The Web interface is intuitive, and results are both easy to understand and visually attractive. Individuals can choose to create a personal account maintained on the website or use the site via a guest account. The privacy statement for the website stipulates that individuals who create an account remain guardians of the data, meaning that account creators control all access. However, individuals using this site should read and review the privacy statement before setting up a personal account.25 Myriad Genetics makes no statements regarding the product’s efficacy or bias.
Paper-based instruments are an effective alternative if online access or privacy is a concern. Several such instruments are available. Hughes et al26 successfully deployed a self-administered paper-based FH instrument for patients in an internal medicine practice, resulting in 6% (51/567) being referred for additional services because of high risks suggested by the FH. A Family History Collection Form created by the National Coalition for Health Professional Education in Genetics is available for download and use.27 The download site includes supplementary instructions for completing and interpreting the collected data.
Barriers for providers and patients
According to HCPs, barriers to performing an FH review include a lack of familiarity with screening recommendations for inherited cancers and a lack of knowledge regarding which patients to refer to geneticists.13 Evidence suggests that low-risk, affluent women are over-referred for genetic counseling and genetic screening tests,28,29 whereas minorities are disproportionately under-referred for these same services.30 Over-referral for genetic testing of low- to average-risk women is associated with use of patient inquiry about FH as a determinant in the decision to refer for genetic screening.29 Barriers to routine collection of FH information also include low patient reading level and privacy concerns. Special efforts may need to be extended to women with low literacy. Some cultural groups may find “keeping it on paper” problematic.31 Protocols and education programs about protections provided by the Genetic Information Nondiscrimination Act will need to be developed and communicated broadly.
Recommendations for risk assessment and referral
In an FH, presence of any of these indicators is a red flag that warrants further investigation and possible referral to a genetics counselor32:
- Several family members with the same or related cancers
- Early age of onset for cancer
- Male breast cancer
- Ashkenazi Jewish descent
The American College [now Congress] of Obstetricians and Gynecologists (ACOG) recommends genetic counseling and screening for unaffected women with a close relative who has been diagnosed with ovarian cancer or a BRCA1/2 mutation.33 In addition, women who have male relatives with breast cancer, multiple cases of breast cancer among close relatives, or close relatives diagnosed with breast cancer at an early age should be offered genetic screening.33 The most recent screening/genetics referral recommendations by the National Comprehensive Cancer Network are similar to those of ACOG, with an additional recommendation to offer genetic risk assessment for unaffected individuals who have more than one family member on the same side affected by any of these cancers: endometrial cancer, pancreatic cancer, aggressive prostate cancer, brain tumors, leukemia/lymphoma, thyroid cancer, or diffuse gastrointestinal cancer.34
Implementation
Under the Affordable Care Act, coverage was extended for preventive health services, including genetic counseling and BRCA testing if a woman’s FH shows evidence of risk for deleterious mutations.35 Commencement of screening for cervical cancer is an opportune time to introduce the idea of FH data collection to young women. A few minutes could be used to discuss the benefits of FH awareness and to present options for data collection (online or paper tool). Women can choose to begin collecting FH data prior to their next scheduled annual visit, which will allow them and their families to discuss family members’ health histories and have adequate time to gather missing details. Interventions and screening should start early; beginning the process in a woman’s early 20s allows adequate time to collect information, determine risk, and, if necessary, refer for screening.
Conclusion
The information and resources provided in this article are intended to facilitate collection and interpretation of the FH during the annual well-woman visit. Hereditary patterns of disease are most readily identified by review of a comprehensive FH. As such, HCPs need to develop skills in collecting and interpreting FHs. Improved collection and documentation skills for HCPs may have a profound impact on decisions about further screening, disease prevention, and treatment options for inherited cancer.
Mary Elizabeth “Betsy” Guimond is Assistant Professor of Nursing at Robert Morris University in Pittsburgh, Pennsylvania. The author states that she does not have a financial interest in or other relationship with any commercial product named in this article.
Suggested reading
Cancer Genetics Risk Assessment and Counseling–for health professionals (PDQ®). Updated July 17, 2015. cancer.gov/about-cancer/causes-prevention/genetics/risk-assessment-pdq
References
1. van Altena AM, van Aarle S, Kiemeney LA, et al. Adequacy of family history taking in ovarian cancer patients: a population-based study. Fam Cancer. 2012;11(3):343-349.
2. Nilsson MP, Hartman L, Idvall I, et al. Long-term prognosis of early-onset breast cancer in a population-based cohort with a known BRCA1/2 mutation status. Breast Cancer Res Treatment. 2014;144(1):133-142.
3. Yoshida K, Miki Y. Role of BRCA1 and BRCA2 as regulators of DNA repair, transcription, and cell cycle in response to DNA damage. Cancer Science. 2004;95(11):866-871.
4. Petrucelli N, Daly MB, Feldman GL. BRCA1 and BRCA2 hereditary breast and ovarian cancer. GeneReviews®. 2013. ncbi.nlm.nih.gov/books/NBK1247/
5. Woodson AH, Profato JL, Muse KI, Litton JK. Breast cancer in the young: role of the geneticist. J Thorac Dis. 2013;(5 suppl 1):S19-S26.
6. Vasen HF. Clinical description of the Lynch syndrome [hereditary nonpolyposis colorectal cancer (HNPCC)]. Fam Cancer. 2005;4(3):219-225.
7. Auranen A, Joutsiniemi T. A systematic review of gynecological cancer surveillance in women belonging to hereditary nonpolyposis colorectal cancer (Lynch syndrome) families. Acta Obstet Gynecol Scand. 2011; 90(5):437-444.
8. Lu K, Daniels M. Endometrial and ovarian cancer in women with Lynch syndrome: update in screening and prevention. Fam Cancer. 2013; 12(2):273-277.
9. Kohlmann W, Gruber SB. Lynch syndrome. In: Pagon RA, Adam MP, Ardinger HH, et al, eds. GeneReviews®. Seattle, WA: University of Washington; 2014.
10. Savage KI, Matchett KB, Barros EM, et al. BRCA1 deficiency exacerbates estrogen-induced DNA damage and genomic instability. Cancer Res. 2014;74(10):2773-2784.
11. Finch APM, Lubinski J, Møller P, et al. Impact of oophorectomy on cancer incidence and mortality in women with a BRCA1 or BRCA2 mutation. J Clin Oncol. 2014;32(15):1547-1553.
12. Berliner J, Fay A, Cummings S, et al. NSGC practice guideline: risk assessment and genetic counseling for hereditary breast and ovarian cancer. J Genet Couns. 2013;22(2):155-163.
13. Wood ME, Stockdale A, Flynn BS. Interviews with primary care physicians regarding taking and interpreting the cancer family history. Fam Pract. 2008;25(5):334-340.
14. Vogel TJ, Stoops K, Bennett RL, et al. A self-administered family history questionnaire improves identification of women who warrant referral to genetic counseling for hereditary cancer risk. Gynecol Oncol. 2012;125(3):693-698.
15. Armel SR, McCuaig J, Finch A, et al. The effectiveness of family history questionnaires in cancer genetic counseling. J Genet Couns. 2009; 18(4):366-378.
16. Carmona RH, Wattendorf DJ. Personalizing prevention: the US Surgeon General’s family history initiative. Am Fam Physician. 2005;71(1):36-39.
17. Owens K, Marvin M, Gelehrter T, et al. Clinical use of the surgeon general’s “My Family Health Portrait” (MFHP) tool: opinions of future health care providers. J Genet Couns. 2011;20(5):510-525.
18. Flynn B, Wood M, Ashikaga T, et al. Primary care physicians’ use of family history for cancer risk assessment. BMC Fam Pract. 2010;11(1):45.
19. U.S. Surgeon General. My family health portrait. U.S. Department of Health & Human Services, Office of the Surgeon General; 2007.
20. Facio FM, Feero WG, Linn A, et al. Validation of My Family Health Portrait for six common heritable conditions. Genet Med. 2010;12(6):370-375.
21. Rubinstein WS, Acheson LS, O’Neill SM, et al. Clinical utility of family history for cancer screening and referral in primary care: a report from the Family Healthware Impact Trial. Genet Med. 2011;13(11):956-965.
22. Centers for Disease Control and Prevention. Public Health Genomics. Family History. Family History Collection Tools. Family healthware™. June 20, 2013. cdc.gov/genomics/famhistory/resources/tools.htm
23. Myriad Genetic Laboratories. Heriditary Cancer Quiz™. 2014. hereditarycancerquiz.com/
24. Myriad Genetic Laboratories. Family History Tool™. fht.myriad.com/app/#/get-started
25. Myriad Genetic Laboratories. Terms of Use/Privacy policy. fht.myriad.com/app/#/terms
26. Hughes KS, Roche C, Campbell CT, et al. Prevalence of family history of breast and ovarian cancer in a single primary care practice using a self-administered questionnaire. Breast J. 2003;9(1):19-25.
27. National Coalition for Health Professional Education in Genetics. The Jackson Laboratory. Family History Tool. 2014. nchpeg.org/index.php?option=com_content&view=article&id=61&Itemid=74.
28. White DB, Bonham VL, Jenkins J, et al. Too many referrals of low-risk women for BRCA1/2 genetic services by family physicians. Cancer Epidemiol Biomarkers Prev. 2008;17(11): 2980-2986.
29. Bellcross CA, Kolor K, Goddard KA, et al. Awareness and utilization of BRCA1/2 testing among U.S. primary care physicians. Am J Prev Med. 2011;40(1):61-66.
30. Trivers KF, Baldwin LM, Miller JW, et al. Reported referral for genetic counseling or BRCA 1/2 testing among United States physicians: a vignette-based study. Cancer. 2011; 117(23):5334-5343.
31. Thompson T, Seo J, Griffith J, et al. “You don’t have to keep everything on paper”: African American women’s use of family health history tools. J Community Genet. 2013;4(2):251-261.
32. National Coalition for Health Professional Education in Genetics. The Jackson Laboratory. Interpreting the Family History. 2014. nchpeg.org/index.php?option=com_content&view=article&id=170&Itemid=64
33. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 103: Hereditary breast and ovarian cancer syndrome. Obstet Gynecol. 2009;113(4):957-966.
34. Daly MB, Pilarski R, Axilbund JE, et al. Genetic/familial high-risk assessment: breast and ovarian, version 1.2014. J Natl Compr Canc Netw. 2014; 12(9):1326-1338.
35. Centers for Medicare & Medicaid Services. Affordable Care Act Implementation FAQs – Set 12. cms.gov/CCIIO/
Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.html
