Increased stress among individuals during pregnancy and postpartum is an important mental health concern. The most common stressors during pregnancy and postpartum include social support, low quality of life including physical health, psychologic status, social relationships, and environmental conditions.1 Anxiety and depression continue to be the most common mental health conditions experienced during pregnancy.2 It is estimated that between 20% and 40% of women experience symptoms of depression or anxiety during pregnancy.3 According to the Centers for Disease Control and Prevention (CDC), 1 in 8 women experience depression following birth and the incidence is on the rise.4 Suicide is the leading cause of maternal death in developed countries during pregnancy and in the 12 months following birth, and suicidal ideation varies in pregnancy between 2.6% and 29.2%.5,6 According to the CDC, 10% of pregnant persons used alcohol and, of this number, at least 40% used another substance, most commonly tobacco and marijuana.7 A similar study indicated more than half of pregnant persons who used opioids for nonmedical reasons drank more than five alcoholic drinks per day.7 Over 60% of parents report burnout, with female gender having a significant increased risk.8 Parental burnout has been strongly associated with increased depression, anxiety, and alcohol consumption, and negative reactions such as insulting, criticizing, yelling, cursing at, and/or physically harming their children.8
Nurse practitioners (NPs) can facilitate positive mental health outcomes by incorporating an evidence-based, collaborative, person-centered guiding psychotherapy approach called motivational interviewing (MI) to help patients improve self-care habits such as abstinence from harmful substance use and stress management during pregnancy and postpartum. The purpose of this article is to provide NPs with tools and strategies to implement MI in any patient encounter with a goal of promoting self-care activities that can improve mental health and decrease stress. The focus is pregnancy and postpartum periods. Examples of using MI to promote selected mental health-related self-care behaviors are provided.
Self-care definitions
The World Health Organization defines self-care as the capability of an individual, family, or community to promote and maintain health, prevent disease, and cope with illness and disability, all with or without the involvement of a healthcare provider.9 There are many forms of evidence-based self-care strategies: exercise; reducing and/or abstaining from tobacco, alcohol, and illicit substances; meditation; mindfulness; reading; massage therapy; sleep hygiene; relationship support; support groups; and reducing stress around breastfeeding. The evidence for MI with self-care behaviors shows improved outcomes related to breastfeeding promotion, tobacco abstinence, managing depression, diet, and exercise as key target areas for both maternal and infant health.10
Motivational interviewing definitions
Motivational interviewing is defined as an evidence-based, collaborative, person-centered guiding approach to initiating motivation for positive health change.11 The overarching goal of MI is to inspire the patient to increase their intrinsic motivation to change versus persuaded change from external sources.11 Having a paternalistic approach is not effective to lead patients to positive behavior change and therefore having the patient determine the “why” is one of the initial strategies in MI. The traditional approach of the “righting reflex” by telling patients to change, what to change, and how to change can often lead to change resistance.12 In 1983, MI was initially applied to treat alcohol use disorders and is now widely employed in treatment for drug use, gambling, eating disorders, and anxiety disorders, for chronic disease management, and for facilitating health-related behavior changes.11 It is used to promote health by offering strategies and tools that support positive self-care behaviors. Evidence strongly supports MI as an effective therapy to improve lifestyle behaviors prepregnancy and during pregnancy that include self-reported reduction in smoking and alcohol consumption.13 Clinical trial evidence shows benefit in promoting dietary changes and weight management.12 Nurse practitioners can easily implement MI during any prenatal or postpartum patient encounter.
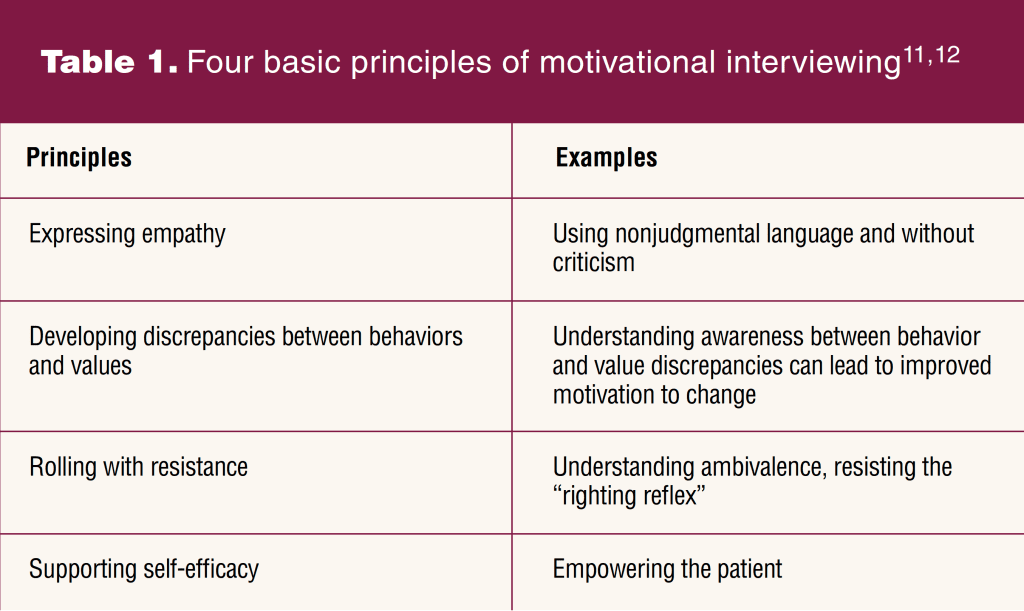
Principles of motivational interviewing
There are four basic principles of MI: expressing empathy, developing discrepancies between behaviors and values, rolling with resistance, and supporting self-efficacy as described in Table 1.11,12 A variety of evidence-based strategies are available to NPs to facilitate each principle in practice and can be utilized throughout every step of the process.11
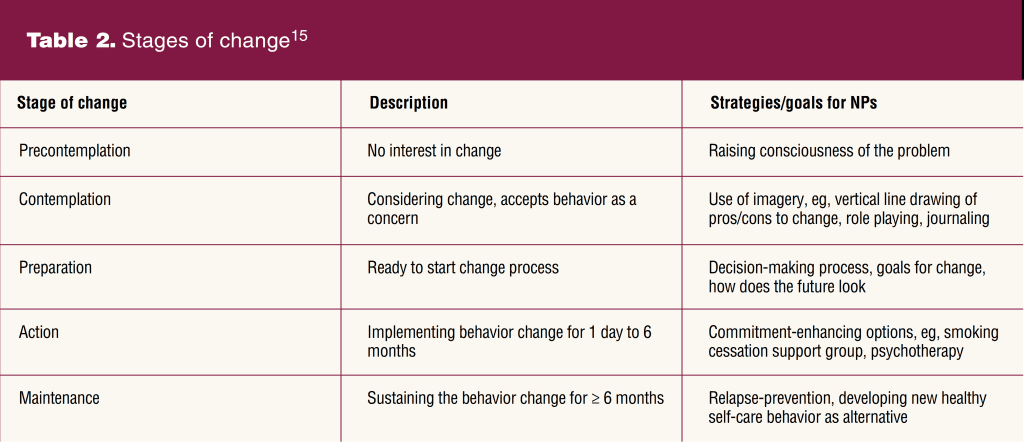
Stages of change with motivational interviewing
It is important for NPs to understand how the stages of change are intertwined within MI, which is often referred to as “change talk.”10 MI incorporates addressing perceived barriers to the change, implementing strategies to overcome the barriers, providing additional counseling during the change, and grouping change phases together.14 Change often ebbs and flows through five recognized stages including precontemplation, contemplation, preparation, action, and maintenance as described in Table 2.11,15 The NP should consider these stages prior to initiating MI techniques during patient encounters and meet the patient where they are in the process.
Change talk
MI is divided into two primary phases: the ambivalence phase, which aligns with the contemplation stage of change, and the readiness phase, which aligns with the preparation and action stages of change.11 In the ambivalence phase, the patient is unsure how they feel about the change and motivation alone is likely not enough to accomplish the change. The goal of the NP in this phase is to help resolve the ambivalence associated with the change and build internal drive to motivate the change.11,12 In the readiness phase, the patient shows signs of readiness to change and the NP role is to strengthen the commitment to change and provide education and strategies to implement the change plan.11
Change talk with MI requires NPs to evaluate contemplation, asking open-ended questions, listening reflectively, providing affirmations, summarizing goals, and planning consequent visits. It is helpful to remember the following tips: first, select a primary target behavior for change. Evidence suggests that pursuing one behavior change at a time results in the best response in achieving a target goal.12 Second, use open-ended questions; examples can be described using the DARN-CAT (Desire, Ability, Reasons for change, Need and Commitment, Action Taken) mnemonic for recognizing and mobilizing change.12 Using this mnemonic, NPs can determine if the patient makes “preparatory or mobilizing” statements.12 If the NP determines the patient has preparatory type statements, specific questions include:
- How do you feel about changing? What is your desire for this change?
- What are some strategies that you may be able to include in this change?
- What are some reasons you want to change?
- What is the need for you to make this change? Using the ruler method to assess the need is a useful way to assess and evoke change: on a scale from 0 to 10 (0 meaning not at all, 10 meaning extremely important) how important is changing this right now?
If the patient is using mobilizing change talk, ask questions such as:
- What is your commitment to changing?
- What actions might you take to start this change?
- What steps have you already taken toward making this change?
Four processes in the approach to motivational interviewing
There are four processes to consider in the approach to MI during the patient encounter: engaging, focusing, evoking, and planning. During the engaging process, the NP focuses on establishing a collaborative relationship.12 It is important for the NP to ask permission prior to giving advice when performing MI. The focusing phase develops a specific emphasis and direction. The evoking phase involves the patient describing their motivation to change and how it should occur, followed by the planning phase during which the specifics will develop on how and when the change will occur.12
The two primary goals throughout the four processes of the MI approach include establishing the “spirit of MI” and using the “method of MI.”12 The spirit of MI involves collaboration, acceptance, compassion, and elicitation.12,16 It is important the NP and patient work as partners through the process. The NP should accept the patient as they are while using compassion and empathy. Finally, the NP needs to focus on elicitation, through which the NP acknowledges the patient has the knowledge and skills they need to make the change while aiding their motivation and commitment.12
The specific techniques utilized by the NP to aid MI are described as the method of MI.11 They can use specific interviewing techniques to facilitate discussion with a goal for the patient to verbalize change talk.12 An example of method of MI includes using the OARS mnemonic: asking Open-ended questions, Affirming patient ideas about the change process, listening Reflectively, and Summarizing the information.11,12 Open-ended questions facilitate an infinite set of potential responses (eg, “How do you feel about your alcohol use?”). Affirmations include NP statements that address the positivity behind the efforts (eg, “You have worked hard to decrease your salt intake.”). Reflective listening can include simple statements such as “You do not like dealing with your gestational diabetes” or complex statements such as “You feel like your diet is out of your control.” Both statements can provide reassurance the NP is actively listening, and complex statements add that the NP understands the meaning behind the patient’s words.12
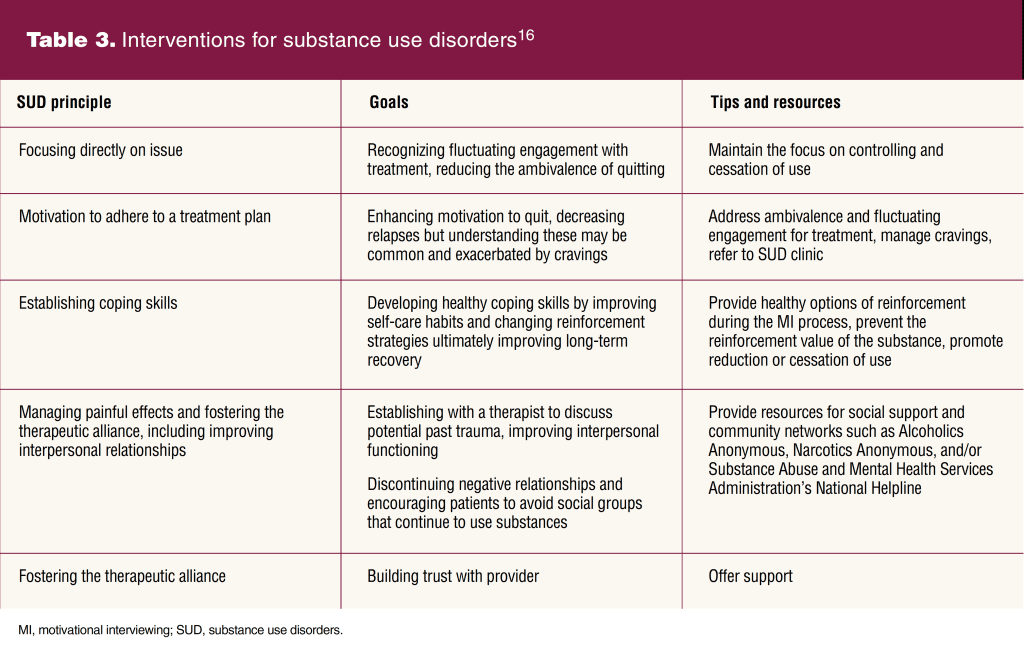
Motivational interviewing and self-care behaviors for substance use disorders
Substance use disorders (SUDs) are often listed as the most significant physical and mental health concern during pregnancy and postpartum. Motivational interviewing has been shown to be an effective method for reducing and abstaining from harmful substances in multiple randomized controlled trials, with the strongest evidence for tobacco and alcohol use.16 Specific management strategies NPs can use for MI with SUDs during pregnancy and postpartum focus directly on the principles identified in Table 3.16 Evidence supports the most benefit with three or more MI sessions between the early prenatal period and 12 months’ postpartum.10
Motivational interviewing and self-care for stress management
The need for stress management is often identified with motivational interviewing. Effective self-care interventions that can be encouraged for reducing stress include mindfulness and meditation (MM). Strategies for MM include activities such as: yoga, deep abdominal breathing techniques, daily meditation, guided imagery, massage therapy, and psychotherapy. Outcomes of MM interventions used during pregnancy and postpartum include significantly less stress, lower self-reports of depression and anxiety, decreased sleep disturbances, and improved self-efficacy.17,18 Several studies identified in a systematic review demonstrated the positive effect of yoga on decreasing anxiety, depression, and stress during pregnancy.19 Yoga has been shown to improve interoceptive awareness, which may help develop coping skills and reduce overall stress.19 These MM practices also have been shown to be helpful in self-care behaviors for management of SUDs.17,18,20
Evidence supports the use of phone applications (apps) for MM due to ease of use, less resources for delivery, and increased access.21 Specific examples of these apps are Calm, Peloton, Headspace, Mind the Bump, Expectful, Insight Timer, Sanity & Self, and Smiling Mind. Using the Expectful app, researchers found the average Perceived Stress Scale score among pregnant participants was significantly lower in the group using the app at 28 weeks’ gestation.18
Addressing barriers to change
Barriers identified include time constraints, poor baseline knowledge, family culture, food accessibility, and lack of relevant data sources.22 Additional barriers may be present related to SUDs including stigma and underlying mental health concerns. Using persuasion, offering unsolicited advice, and confrontation may impede MI success.12 Persuasion includes giving biased information, sharing concerns, and giving tips or solutions without permission.12 Confrontation includes any approach that is judgmental, negative, disapproving, or argumentative.12 Nurse practitioners can intervene by performing MI using the aforementioned tips and technique, addressing the barriers, and providing evidence-based strategies and resources.
Conclusion and implications for practice
Motivational interviewing is a flexible, individualized, easily incorporated care approach that NPs can use to promote positive self-care behavior among patients, particularly during pregnancy and postpartum. It is an evidence-based form of psychotherapy used across a broad spectrum of clinical settings and patient populations. The description of basic MI principles and processes in this article including examples, strategies, and goals can be readily applied to patients who are pregnant or postpartum. Discussions initiated by NPs to promote healthy lifestyle behaviors should occur at every prenatal and postpartum visit. These discussions should incorporate MI and include specific evidence-based strategies to impact meaningful, measurable, and positive self-care behavior change. The use of MI to support reduction and abstinence from harmful substances, and stress management with mindfulness and meditation can help patients achieve self-care goals to improve both mental and physical health outcomes for themselves, their children, and their families. Nurse practitioners have an opportunity to provide MI in all clinical settings to help initiate change in behavior to promote healthier pregnancy and postpartum outcomes.
Shannon L. Linder is Assistant Clinical Professor and Randee Masciola is Associate Clinical Professor at The Ohio State University-College of Nursing in Columbus, Ohio. The authors have no actual or potential conflicts of interest in relation to the contents of this article.
Womens Healthcare. 2023;11(3):20-25. doi: 10.51256/WHC062320
References
1 Kashanian M, Faghankhani M, YousefzadehRoshan M, et al. Woman’s perceived stress during pregnancy; stressors and pregnancy adverse outcomes. J Maternal-Fetal Neonatal Med. 2021;34(2):207-215.
2 Saad A, Magwood O, Aubry T, et al. Mobile interventions targeting common mental disorders among pregnant and postpartum women: an equity-focused systematic review. Demidenko E, ed. PLoS ONE. 2021;16(10):e0259474.
3 Wallace K, Araji S. An overview of maternal anxiety during pregnancy and the post-partum period. J Ment Health Clin Psychol. 2020;4(4):47-56.
4 Centers for Disease Control and Prevention. Identifying maternal depression: missed opportunities to support moms. May 2020. https://www.cdc.gov/reproductivehealth/vital-signs/identifying-maternal-depression/VS-May-2020-Maternal-Depression_h.pdf.
5 Chin K, Wendt A, Bennett IM, Bhat A. Suicide and maternal mortality. Curr Psychiatry Rep. 2022;24(4):239-275.
6 Legazpi PCC, Rodríguez-Muñoz MF, Olivares-Crespo ME, Izquierdo-Méndez N. Review of suicidal ideation during pregnancy: risk factors, prevalence, assessment instruments and consequences. Psicol Refl Crít. 2022;35(1):13.
7 Centers for Disease Control and Prevention. Polysubstance use during pregnancy. September 19, 2022. https://www.cdc.gov/pregnancy/polysubstance-use-in-pregnancy.html.
8 Gawlik K, Melnyk B, Mazurek K. Pandemic Parenting: Examining the Epidemic of Working Parental Burnout and Strategies to Help. Published online May 2022. https://wellness.osu.edu/sites/default/files/documents/2022/05/OCWO_ParentalBurnout_3674200_Report_FINAL.pdf.
9 World Health Organization. WHO Guideline on Self-Care Interventions for Health and Well-Being. 2022 rev. World Health Organization; 2022.
10 Gregory EF, Maddox AI, Levine LD, et al. Motivational interviewing to promote interconception health: a scoping review of evidence from clinical trials. Patient Educ Couns. 2022;105(11):3204-3212.
11 Arkowitz H, Miller WR, Rollnick S, eds. Motivational Interviewing in the Treatment of Psychological Problems, 2nd ed. Guilford Press; 2017.
12 Tooley EM, Kolahi A. Motivating behavioral change. Med Clin North Am. 2022;106(4):627-639.
13 van der Windt M, van Zundert SKM, Schoenmakers S, et al. Effective psychological therapies to improve lifestyle behaviors in (pre)pregnant women: a systematic review. Prev Med Rep. 2021;24:101631.
14 Boom SM, Oberink R, Zonneveld AJE, et al. Implementation of motivational interviewing in the general practice setting: a qualitative study. BMC Prim Care. 2022;23(1):21.
15 Wheeler K. Psychotherapy for the Advanced Practice Psychiatric Nurse: A How-To Guide for Evidence-Based Practice, 3rd ed. Springer; 2020.
16 Herron AJ, Brennan T, American Society of Addiction Medicine, eds. The ASAM Essentials of Addiction Medicine, 3rd ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2020.
17 Smith RB, Mahnert ND, Foote J, et al. Mindfulness effects in obstetric and gynecology patients during the coronavirus disease 2019 (COVID-19) pandemic: a randomized controlled trial. Obstet Gynecol. 2021;137(6):1032-1040.
18 Porter AC, Hunter S, Noonan K, Hoffman MC. A mindfulness application for reducing prenatal stress. J Midwifery Womens Health. 2022;67(4):442-447.
19 Villar-Alises O, Martinez-Miranda P, Martinez-Calderon J. Prenatal yoga-based interventions may improve mental health during pregnancy: an overview of systematic reviews with meta-analysis. Int J Environ Res Public Health. 2023;20(2):1556.
20 Babbar S, Oyarzabal AJ, Oyarzabal EA. Meditation and mindfulness in pregnancy and postpartum: a review of the evidence. Clin Obstet Gynecol. 2021;64(3):661-682.
21 Sandborg J, Henriksson P, Larsen E, et al. Participants’ engagement and satisfaction with a smartphone app intended to support healthy weight gain, diet, and physical activity during pregnancy: qualitative study within the HealthyMoms trial. JMIR Mhealth Uhealth. 2021;9(3):e26159.
22 Ku CW, Leow SH, Ong LS, et al. Developing a lifestyle intervention program for overweight or obese preconception, pregnant and postpartum women using qualitative methods. Sci Rep. 2022;12(1):2511.
Key words: prenatal, postpartum, self-care, physical activity, mental health, women’s health, motivational interviewing, lifestyle interventions, reproductive health