The National Association of Nurse Practitioners in Women’s Health (NPWH) asserts that a trauma-informed approach to delivery of healthcare is essential. Current or past experiences of trauma can have a powerful influence on all aspects of an individual’s health and wellbeing. Knowledgeable and skilled women’s health nurse practitioners (WHNPs) and other advanced practice registered nurses that provide women’s and gender-related healthcare are key to creating physically and emotionally safe environments for patients and staff, recognizing signs and symptoms of trauma, and providing opportunities for trauma survivors to build a sense of control and empowerment through recognizing resilience and avoiding stigmatization. NPWH supports the inclusion of trauma-informed care (TIC) content in nurse practitioner education program curricula, training of all healthcare providers and staff for a trauma-informed workforce, and clinical and organizational policies that reflect a commitment at all levels of the healthcare system to operationalize a TIC approach.
Addressing trauma takes a public health approach that includes public education and awareness, prevention and early intervention, and effective trauma-specific assessment and treatment.1 NPWH advocates for federal, state, and local policies and funding that enhance trauma prevention and increase the availability of resources needed by trauma survivors. Further, NPWH recognizes the need for ongoing research to improve strategies for trauma prevention, promote best practices for trauma-informed care for all settings and populations, and establish effective therapies for healing and recovery.
Background
Trauma includes any experience that causes an intense psychological or physical stress reaction. Trauma can result from an event, series of events, or set of circumstances. Trauma experiences can be current, ongoing, or associated with remote events of childhood. The adverse effects can influence all aspects of an individual’s wellbeing.1 Traumatic events may include childhood abuse or neglect, intimate partner violence, sexual assault, repeated or sustained discrimination, adverse birth experiences, natural disasters, wars, separation from family, and other physically or emotionally harmful experiences. A critical element that defines an event as a traumatic experience is the individual’s subjective response. Not all individuals exposed to trauma experience long-term health problems. This may be due partly to supportive environments, positive coping skills, and available therapeutic resources.1–3 When an individual who experiences trauma does not have access (personally, situationally) to adaptive coping mechanisms and healing resources, they may experience ongoing stress and resort to maladaptive behaviors to cope.1–3
A range of mental and physical health conditions and socioeconomic challenges are associated with trauma. Mental health conditions associated with trauma include anxiety, depression, posttraumatic stress disorder, substance use disorders, and suicide attempts.3–7 A history of trauma has been associated with increased risk for chronic medical conditions including cardiovascular, lung, liver, and autoimmune disease and cancer.3–7 Trauma survivors may have difficulty in establishing and maintaining healthy and fulfilling relationships and may struggle with achieving stable working and living environments.1,2,7
Trauma has no boundaries and can affect anyone. Members of populations exposed to repeated discrimination and stigmatization at individual and systemic levels, however, including people from ethnic and racial minority groups; lesbian, gay, bisexual, transgender, and queer or questioning (LGBTQ) individuals; individuals with disabilities; individuals living in larger bodies; and people living in low-income communities are disproportionately represented. Structural and social inequities place them in circumstances and environments where there is an increased risk of exposure to trauma and an increased risk for repeated traumatic experiences. They may face adversities that complicate recovery and incur significant challenges to access services that meet their specific needs.3,8–11
Trauma can be particularly harmful when it occurs during childhood. Adverse childhood experiences (ACEs) are a significant and common cause of trauma. ACEs are those which undermine a sense of safety, stability, and bonding (eg, experiencing abuse or neglect; witnessing violence in the home or community; growing up in households with mental health and substance use disorders; parental separation, incarceration of household members). ACEs were first recognized as having a relationship with many of the leading causes of morbidity and mortality in adults in the landmark ACEs study in 1998.4,12 Since 1998, studies have confirmed that ACEs causing toxic (prolonged) stress can negatively affect brain development, immune systems, and stress-response systems leading to health and social problems across the lifespan.5–7 In one study, over 60% of adults reported experiencing at least one ACE and nearly 1 in 6 adults reported four or more types of ACEs.7 Racial and ethnic inequities exist, with American Indian/Alaska Native, Black, and Hispanic individuals more likely to have experienced multiple ACEs than White individuals. Women are more likely than men to have experienced multiple ACEs.4,12 LGBTQ individuals are more likely to have experienced multiple ACEs than the general population.11,13
Trauma survivors may suffer an array of symptoms including anxiety, fearfulness, irritability, emotional swings, agitation, outbursts of anger, and hyperarousal. They may have difficulty concentrating; sleep disturbances; flashbacks (re-experiencing the trauma); difficulty trusting; and feelings of self-blame, guilt, shame, and disconnectedness. Trauma survivors may avoid regular preventive care services because of negative experiences in healthcare interactions that include feelings of stigmatization, bias, discrimination, and re-traumatization. Their symptoms and negative experiences in healthcare interactions can make them feel helpless, insecure, and vulnerable.1,2
Failure to consider a history of trauma when providing healthcare can lead to misdiagnosis, poor treatment outcomes, and ineffective therapeutic relationships.14 A number of experiences in the healthcare setting can be re-traumatizing to the trauma survivor. Examples include being touched unexpectedly or without permission, being instructed to remove clothing, and particular sights, sounds, or odors. When the healthcare provider is not aware of a patient’s trauma experience, they may unknowingly trigger trauma symptoms.1,2
Trauma-informed healthcare approach
A TIC approach acknowledges that many have experienced or witnessed traumatic events and that this can continue to affect aspects of their lives and how they access and experience healthcare.14 Every patient is a potential trauma survivor, so all encounters should be trauma informed.1,14,15 A TIC approach is grounded in an understanding of and responsiveness to the effects of trauma and emphasizes physical, psychological, and emotional safety for survivors, significant others of survivors, and clinicians, staff, and students providing care. It creates opportunities for survivors to build a sense of control and empowerment. Consent is critical in all aspects of TIC including discussion of sensitive topics and physical examination components. A TIC approach also is strength based, recognizes resilience, and avoids stigmatization.1,2,16 As well, TIC can improve healthcare engagement and patient satisfaction.16
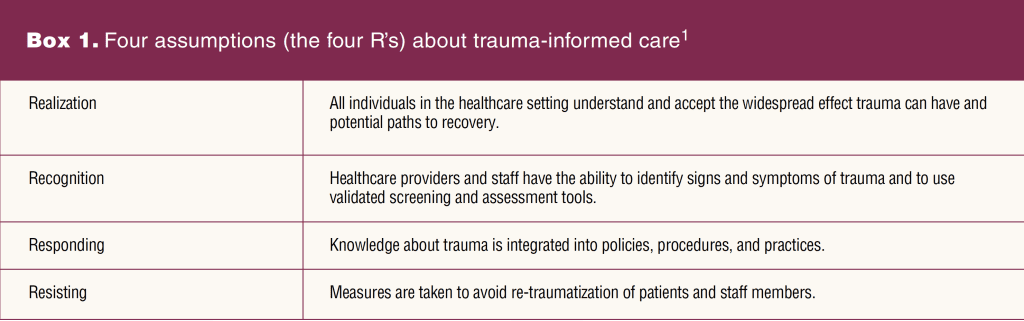
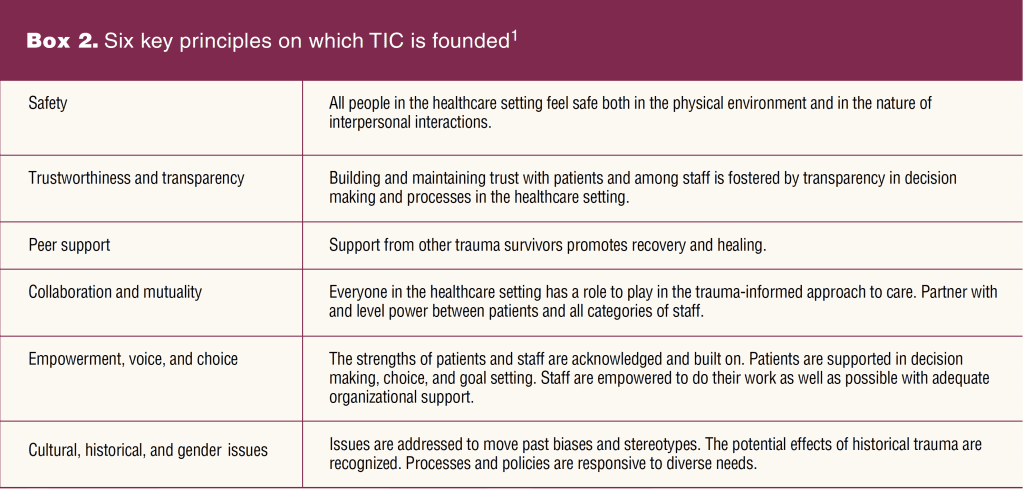
Rather than a set of prescribed practices, healthcare settings, organizations, and systems can use four assumptions (the four “R’s”) outlined by the Substance Abuse and Mental Health Services Administration (SAMHSA) and six key principles to guide implementation of TIC (Box 1, Box 2). Ongoing training and support are needed to implement the four R’s and the six key principles for a TIC approach. A TIC approach is possible and essential in all clinical settings.
Trauma-specific services may or may not be provided in the setting but should be available through referral to specialists in behavioral therapies and other essential aspects of care. Adequate behavioral health providers with expertise in TIC are needed to allow referrals for treatment.
Implications for women’s and gender-related health and healthcare
Women are at risk for trauma in many different aspects of their lives from childhood through adulthood. In the United States, about 1 in 4 women (25.1%) have experienced sexual violence, physical violence, and/or stalking by an intimate partner in their lifetime and reported some form of intimate partner violence-related impact.17 Estimates of the prevalence of psychological trauma that results from sexual assault or sexual harassment while the individual was in military service (military sexual trauma) in females range from 26.9% to 41.5%.18,19 Potentially traumatic perinatal events are not uncommon including labor complications, obstetric interventions, operative deliveries, neonatal complications, perinatal loss, and perceived loss of control/sense of autonomy. Up to 44% of patients report that their childbirth was psychologically traumatic.20,21 LGBTQ youth experience trauma at higher rates than their heterosexual, cisgender peers.11,13 Common traumas experienced include bullying, harassment, physical and sexual abuse, stigmatization, and rejection.22
WHNPs and other clinicians who provide women’s and gender-related healthcare have many opportunities to lead in providing TIC. Knowledge and skills to identify signs and symptoms of trauma, use of validated screening and assessment tools, and providing care that avoids re-traumatization and emphasizes individual strengths and resiliency are essential. Leadership can be provided to ensure that all staff are trained in TIC.
Clinicians working in primary care will not necessarily have the expertise to provide specialized interventions that directly address symptoms or conditions that result from traumatic events. An important component of TIC is to develop a robust trauma-informed referral network with specialists skilled in treating trauma survivors who can provide additional services to assist with recovery and healing.1,2
NPWH leadership
NPWH will provide leadership to ensure:
- Continuing education programs and resources are available to support WHNPs and other advanced practice clinicians who provide women’s and gender-related healthcare in providing TIC at clinical, organizational, and healthcare system levels.
- WHNP educational programs have access to evidence-based information on trauma and trauma-informed care including self-care that can be incorporated into curricula.
- Collaborative engagement with other organizations to advocate for federal, state, and local policies and funding that enhance trauma prevention and increase the availability of resources most needed by trauma survivors.
- Research progresses to improve strategies for trauma prevention, promote best practices for TIC for all settings and populations, and establish effective therapies for recovery.
NPWH gratefully acknowledges Lauren Hansen, DNP, MSN, WHNP-BC; Beth Kelsey, EdD, APRN, WHNP-BC; Ginny Moore, DNP, WHNP-BC; Komkwuan P. Paruchabutr, DNP, FNP-BC, WHNP-BC, CNM; Terrie H. Platt, DNP, WHNP-BC; and Heather Quaile, DNP, WHNP-BC, for their contributions as writing group members of this position statement.
Approved by NPWH Board of Directors: November 2, 2022.
References
1 Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma- Informed Approach. HHS Publication No. (SMA) 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014.
2 Substance Abuse and Mental Health Services Administration. Trauma-Informed Care in Behavioral Health Services. Treatment Improvement Protocol (TIP) Series 57. HHS Publication No. (SMA) 13-4801. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014.
3 Trauma-Informed Care Implementation Resource Center. Center for Health Care Strategies. Fact sheet. Understanding the effects of trauma on health. June 2017. https://www.traumainformedcare.chcs.org/resource/understanding-the-effects-of-trauma-on-health.
4 Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. Am J Prev Med. 1998;14(4):245-258.
5 Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356-366.
6 Bellis MA, Hughes K, Ford K, et al. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health. 2019;4(10):e517-e528.
7 Merrick MT, Ford DC, Ports KA, et al. Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention–25 states, 2015–2017. MMWR Morb Mortal Wkly Rep. 2019;68(44):999-1005.
8 Kirkinis K, Pieterse AL, Martin C, et al. Racism, racial discrimination, and trauma: a systematic review of the social science literature. Ethn Health. 2021;26(3):392-412.
9 Polanco-Roman L, Danies A, Anglin DM. Racial discrimination as race-based trauma, coping strategies, and dissociative symptoms among emerging adults. Psychol Trauma. 2016;8(5):609-617.
10 Ramos N. Medical trauma in LGBTQIA youth: adapting trauma-informed affirming clinical practices. Pediatr Ann. 2021;50(9):e379-e383.
11 Schnarrs PW, Stone AL, Salcido R Jr, et al. Differences in adverse childhood experiences (ACEs) and quality of physical and mental health between transgender and cisgender sexual minorities. J Psychiatr Res. 2019;119:1-6.
12 Centers for Disease Control and Prevention. Violence prevention. About the CDC-Kaiser ACE study. Page last reviewed: April 6, 2021. https://www.cdc.gov/violenceprevention/aces/about.html.
13 Austin A, Herrick H, Proescholdbell S. Adverse childhood experiences related to poor adult health among lesbian, gay, and bisexual individuals. Am J Public Health. 2016;106(2):314-320.
14 Quaile H. Trauma-informed care for the primary care provider. Womens Healthcare. 2020;8(4):6-12.
15 National Clinical Training Center for Family Planning. Clinician guide for trauma-informed care. October 2022. https://www.ctcfp.org/sdm_downloads/clinician-guide-for-trauma-informed-care.
16 Varghese L, Emerson A. Trauma-informed care in the primary care setting: an evolutionary analysis. J Am Assoc Nurse Pract. 2022;34(3):465-473.
17 Smith SG, Zhang X, Basile KC, et al. The National Intimate Partner and Sexual Violence Survey: 2015 Data Brief–Updated Release. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, November 2018. https://www.cdc.gov/violenceprevention/pdf/2015data-brief508.pdf.
18 Barth SK, Kimerling RE, Pavao J, et al. Military sexual trauma among recent veterans: correlates of sexual assault and sexual harassment. Am J Prev Med. 2016;50(1):77-86.
19 Wilson LC. The prevalence of military sexual trauma: a meta-analysis. Trauma Violence Abuse. 2018;19(5):584-597.
20 Hollander MH, van Hastenberg E, van Dillen J, et al. Preventing traumatic childbirth experiences: 2192 women’s perceptions and views. Arch Womens Ment Health. 2017;20(4):515-523.
21 White A, Saxer K, Raja S, Hall SL. A trauma-informed approach to postpartum care. Clin Obstet Gynecol. 2022;65(3):550-562.
22 National Child Traumatic Stress Network. LGBTQ youth. www.nctsn.org/what-is-child-trauma/populations-at-risk/lgbtq-youth.