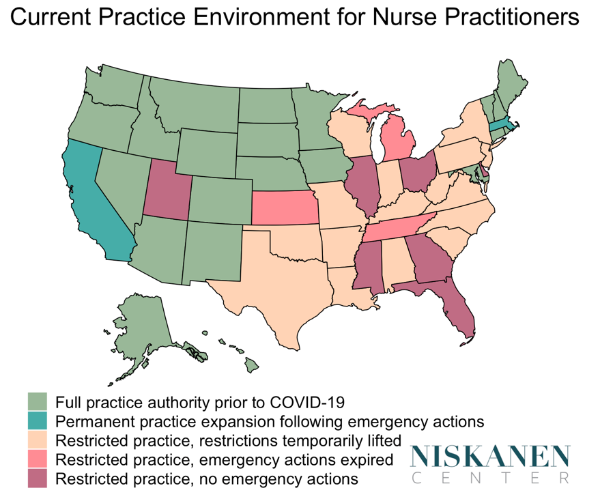
In response to COVID-19, more than 20 states across the country loosened the scope-of-practice restrictions on nurse practitioners (NPs), increasing the capacity of the health care workforce to care for patients. Yet these life-saving measures have generally been left to expire, on the basis of politics rather than evidence. Even before COVID-19, health care workforce capacity was insufficient to meet patient needs. Rolling back scope-of-practice expansion after the crisis is over — let alone now, in its midst — would represent a serious step back for health care access.
Expanding scope of practice for NPs is a tried and tested strategy for improving health care. Before COVID-19, NPs in 22 states could practice safely and independently without physicians looking over their shoulders. NPs are trained to assess, diagnose, and treat patients; prescribe medications; order tests and medical equipment; or admit patients to hospitals for necessary care.
Some state lag behind
Unfortunately, many states have lagged behind on scope of practice reform, requiring that NPs be supervised by physicians or meet extra experience requirements beyond their licensures. For example, New York state requires NPs to have at least 3,600 hours of clinical practice and a “written practice agreement” with a licensed physician consenting to work with them. The surge in health care demand forced many states to reexamine these outdated restrictions. An executive order by Governor Andrew Cuomo permitted NPs to provide health care services appropriate to “their education, training, and experience,” without these agreements and relationships. The executive order also protected NPs from any civil or criminal penalty related to a lack of these agreements. Similar executive orders have been issued by the governors of 23 states. Allowing NPs to care for patients may have saved many lives.
The evidence is clear that NPs deliver high-quality, safe care, and scope-of-practice restrictions only limit NPs’ ability to do so. Many NPs find themselves unable to do their jobs from one day to the next if their collaborating physician retires, dies or loses their license. In our work, we have shown that many physicians in New York state find the unnecessary restrictions burdensome. One physician said, “I’ve asked that many times, ‘Why am I signing for a nurse practitioner who has a Ph.D. and has been working with me since 1998?’ I have absolutely no clue.” These restrictions also prevent patients from quickly accessing health care services.
More NP authority means more access
States granting NPs a greater practice authority experience expanded health care utilization, especially among rural and vulnerable populations. States such as New York have traditionally faced uneven access to primary care providers. In 2019, the ratio of population to primary care physicians across New York state counties ranged from 700:1 to 13,780:1. Millions of New Yorkers, particularly those living in rural, low-income, and minority communities, are without access to primary care. Almost 5 million New Yorkers live in areas that are designated Primary Care Health Professional Shortage Areas. Federally qualified health centers in the state that mostly serve low-income and minority patients are unable to recruit primary care physicians and NPs. And NPs cannot practice in areas without physicians if the state requires agreements between these two health professionals.
NPs can help to meet the growing demand for chronic care services. Evidence shows that NPs are well-suited and uniquely qualified to deliver care to chronically ill patients given their nursing training and a background that focuses on the overall health and well-being of the patient and not on the disease alone. Consider the fact that more than 40 percent of New York adults suffer from a chronic disease. These individuals need timely access to primary care services to manage their conditions. We know that those who suffer chronic health conditions are most at risk for COVID-19; 91.6% percent of all COVID-19 deaths in New York were among people who had underlying chronic illnesses, such as hypertension and diabetes. We are also learning that minorities, who suffer disproportionately from chronic illnesses, have been dying at a disproportionally higher rate from COVID-19.
No need to go back
Governors’ willingness to temporarily lift scope of practice restrictions to begin with demonstrates that such restrictions are arbitrary rather than evidence-based. Even in a crisis, no governor would risk the public’s safety by allowing unqualified clinicians to care for patients without oversight. If NPs are qualified to care for the sickest patients during the most challenging times of crisis and chaos without a physician’s supervision, then they should certainly be able to operate autonomously in normal times.
There is no need to go back to outdated, artificial restrictions as these executive orders expire. Post-COVID-19, more than ever, we will need to optimally use all health care resources, including the growing NP workforce, whose numbers almost doubled from 2010 to 2017 and continue to grow rapidly.
Many more states are considering permanent expansion of the NP scope-of-practice regulations. On January 1, Massachusetts Governor Charlie Baker signed a new law titled “An Act Promoting a Resilient Health Care System That Puts Patients First.” The law enables NPs to practice independently, provided that they meet educational and training requirements. Allowing NPs to deliver care to Americans without restrictions will assure that when disasters happen, Americans will be healthier and more ready to weather them, and our health care system will be prepared.
Lusine Poghosyan is a Stone Foundation and Elise D. Fish Professor of Nursing at Columbia University School of Nursing and Professor of Health Policy and Management at Mailman School of Public Health, Columbia University. She is also the Executive Director of the Center for Healthcare Delivery Research & Innovations (HDRI) at Columbia University.