A trauma-informed care (TIC) approach acknowledges that many have experienced or witnessed traumatic events and that this can continue to affect aspects of their lives and how they access and experience healthcare. Transgender and gender nonconforming (TGNC) individuals are highly represented among those who have experienced trauma, often have gender dysphoria, and face substantial healthcare disparities and barriers to care. A high prevalence of suicide attempts, HIV infection, substance use disorders, and other health inequities affect the TGNC communities. Data suggest that 24% of transgender people experience unequal treatment in healthcare environments, 19% are refused care, and 33% do not seek preventive services. The key to being trauma informed in providing healthcare for TGNC individuals encompasses training of providers and staff, and developing policies and procedures in organizational systems that support TIC.
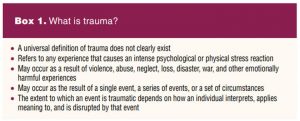 Healthcare providers (HCPs) in any setting will see individuals with a history of trauma. (See Box 1 for the definition of trauma.) It is imperative to have a working knowledge of ways to support these individuals. The connection between trauma, mental health, and co-occurring disorders such as substance abuse, eating disorders, HIV/AIDS, and violence have been well documented.1–3 Further, data have shown that repeated exposure to traumatic events can decrease treatment adherence.1–3 Failure to consider a history of trauma can lead to misdiagnosis, poor treatment outcomes, and ineffective therapeutic relationships.
Healthcare providers (HCPs) in any setting will see individuals with a history of trauma. (See Box 1 for the definition of trauma.) It is imperative to have a working knowledge of ways to support these individuals. The connection between trauma, mental health, and co-occurring disorders such as substance abuse, eating disorders, HIV/AIDS, and violence have been well documented.1–3 Further, data have shown that repeated exposure to traumatic events can decrease treatment adherence.1–3 Failure to consider a history of trauma can lead to misdiagnosis, poor treatment outcomes, and ineffective therapeutic relationships.
The information gleaned in this article builds on information in the articles published in the June 2021 and August 2020 issues of Women’s Healthcare.4,5 In the August 2020 article “Trauma-informed care for the primary care provider,” the author provided an overview of trauma, universal screening, and trauma-informed care (TIC) and discussed the four R’s and six key principles HCPs can use to implement TIC.4 In the June 2021 article “Part 1: The road to operationalizing trauma-informed care,” the authors discussed strategies HCPs can use to implement a trauma-informed approach at the clinical level and organizational level.5 In this article, the author discusses a blueprint for planning and implementing TIC for transgender and gender nonconforming (TGNC) individuals to meet the medical and mental health needs of this underserved and vulnerable population.
Trauma and transgender and gender nonconforming individuals
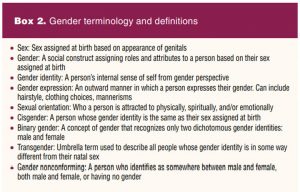 Individuals who experience or express a gender that differs from their sex assigned at birth may identify as TGNC individuals. These identities may include trans feminine (male to female), trans masculine (female to male), and nonbinary identities. Gender-related terminology with definitions is provided in Box 2. In the United States, approximately 150,000 youth and 1.4 million adults identify as transgender.6 This estimate may actually be low considering that TGNC individuals may not disclose their identities due to fear and harassment.6 Negative healthcare experiences are frequently reported by TGNC individuals, and they often avoid seeking healthcare due to fear of discrimination. Among respondents to the 2015 US Transgender Survey, “one-third reported having a negative experience with a healthcare clinician in the past year, including being asked unnecessary or invasive questions, having to teach their clinician in order to get appropriate care, or being refused transition-related care.”6 In the same survey, 19% of respondents reported being refused care altogether and 33% reported not seeking preventive services.6
Individuals who experience or express a gender that differs from their sex assigned at birth may identify as TGNC individuals. These identities may include trans feminine (male to female), trans masculine (female to male), and nonbinary identities. Gender-related terminology with definitions is provided in Box 2. In the United States, approximately 150,000 youth and 1.4 million adults identify as transgender.6 This estimate may actually be low considering that TGNC individuals may not disclose their identities due to fear and harassment.6 Negative healthcare experiences are frequently reported by TGNC individuals, and they often avoid seeking healthcare due to fear of discrimination. Among respondents to the 2015 US Transgender Survey, “one-third reported having a negative experience with a healthcare clinician in the past year, including being asked unnecessary or invasive questions, having to teach their clinician in order to get appropriate care, or being refused transition-related care.”6 In the same survey, 19% of respondents reported being refused care altogether and 33% reported not seeking preventive services.6
TGNC individuals are more likely to experience potentially traumatic events such as physical assault and victimization by acts of prejudice and transphobia, such as misgendering and employment discrimination.6–8 These experiences have negative mental health impacts, contributing to heightened rates of mental health disorders when comparing TGNC and cisgender individuals. TGNC individuals may have gender dysphoria. Gender dysphoria is a sense of anxiety that a person may have because of a discordance between their biologic sex and their gender identity.1 Gender dysphoria manifests early in childhood and can persist for years before patients undergo counseling and treatment. In one study of adult patients seeking gender-affirming surgery, approximately 3 out of 4 participants reported they first experienced gender dysphoria by age 7 years.9 In this same study, transgender women were an average 27.1 years and transgender men 22.9 years before they began social transition and/or hormonal therapy.9 In other words, their life experiences, beginning with their earliest memories, included the distress and negative health effects brought on by a lack of early counseling and support services that would have eased their gender transition period. Untreated gender dysphoria can result in poor quality of life, beginning in childhood and lasting throughout adolescence and adulthood.10 High rates of depression, anxiety, self-harm, and feelings of hopelessness are reported.10
Gender dysphoria can be successfully treated with gender-affirming hormone and/or surgical treatment along with supportive counseling. Gender-affirming care includes an evaluation of the magnitude, duration, and stability of any gender dysphoria.11 Existing or preexisting conditions (eg, depression, body dysmorphic disorder, substance use disorder) may confound the clinical picture and thus must be considered in an evaluation to optimize treatment.11
Implementing trauma-informed care for trans-gender and gender nonconforming individuals into the practice setting
A TIC approach acknowledges that many people have experienced or witnessed traumatic events and that this can continue to affect many aspects of their lives and how they access and experience healthcare. Individuals who have experienced trauma find themselves in healthcare settings that too often re-traumatize them. Learning to interact with those who have experienced trauma in ways that encourage their resiliency and growth is imperative. A TIC approach aims to be sensitive to individuals’ experiences of trauma and how their trauma may affect their healthcare.7,8 Guidelines for TIC emphasize the need for a holistic approach in which all components of an individual’s history and identity are considered in treatment planning and service delivery. To provide competent TIC for patients who are TGNC, it is necessary first for practices to guide themselves through a self-assessment process. Comprehensive training and planning based on three principles is key to promoting understanding and to providing optimal care. The three principles address understanding the impact of trauma on TGNC individuals, providing physical and emotional safety, and adapting practice policies and procedures to maximize inclusion of TGNC individuals and minimize re-traumatization. Detailed guidelines on incorporating these principles are available for trauma-informed practice as well as care specific to TGNC individuals.12
Principle 1. Understand the impact of trauma on a patient’s cognition, emotion, behavior, and perception
The way that we respond and feel about the world is shaped by exposure to trauma. Stigma, rejection by family or peers, and feelings of shame are common trauma experiences for individuals who are TGNC. The ability to form trusting, intimate relationships, manage stress, maintain self-esteem, and achieve self-sufficiency are impacted.11,13,14 These individuals can be at high risk for depression, violence, substance use, sexual risk behaviors, and truancy.11,13,14
When an understanding of trauma is missing in care, patients may be pathologized in a stigmatizing way and this can also lead to misdiagnosis, improper treatment, and poor outcomes.
HCPs who are willing to explore multiple perspectives, recognize and work to eliminate their own biases, and learn more about TIC and the healthcare needs of TGNC individuals can provide compassionate, comprehensive, and high-quality care. They can also support other staff to do the same.11,13,14
Principle 2. Provide physical and emotional safety to ensure trans-gender and gender-diverse individuals’ healthcare needs and concerns are met
People who have experienced trauma are frequently hypervigilant. They are often acutely aware of their environment. If there is any indication that the environment is unsafe, it can be a distraction and may re-traumatize the patient. TGNC individuals who have faced stigma in their families and communities can feel powerless and exploited.15–19 Strategies that establish a safe and welcoming environment are critical in effectively engaging and building a trusting relationship.19 The physical space where care takes place is important and there are several ways providers can help members of the transgender and broader LGBTQ community feel welcome in the clinical setting. Advertising a practice as accepting of members of the LGBTQ community is imperative. Materials specifically designed and displayed for TGNC populations should be visible and can include posters, brochures, rainbow flags, and flyers about LGBTQ-themed community events. Bathrooms need to have locks and be gender appropriate/neutral.20–24 Intake forms can be updated to include gender-neutral language and asking two questions to identify chosen gender identity and sex assigned at birth to help identify transgender patients, with each patient having the ability to withhold this information if they so choose. Staff and HCPs should be comfortable in discussing sexual orientation, gender identity, and sexual practices. Emotional safety is promoted when care is nonjudgmental, patient centered, and strengths based. This includes open-ended questions, active listening, and affirmations by the HCP. Gender-affirming language that includes the use of preferred pronouns is essential in creating a welcoming environment in which marginalized people feel seen in a holistic and respectful manner.15,16
It is essential to discuss the support and safety of the patient’s social environment as it pertains to gender affirmation. Many TGNC individuals have suffered years of abuse, neglect, or exploitation, and they may have lacked role models for healthy relationships.11,17,19,25 HCPs can provide a valuable opportunity for patients to examine their relationship history, discuss healthy, safe intimate relationships, and offer referrals where needed. When issues around gender identity are avoided, more individuals are unprepared to navigate these complexities, which can compound shame. HCPs should be equipped to handle the basic mental health needs of TGNC individuals and refer to specialists when needed. TGNC patients typically have high rates of mental health diagnoses. However, it is import-ant not to assume that a patient’s mental health concerns are secondary to being transgender. HCPs should consider routine screening for depression, anxiety, posttraumatic stress disorder, eating disorders, substance use, intimate partner violence, self-injury, bullying, truancy, homelessness, high-risk sexual behaviors, and suicidality. Gender dysphoria and past negative experiences can cause significant distress for TGNC patients during the physical examination. Examinations should be based on the patient’s specific needs for the visit. Prior to a genital exam, the HCP should ascertain if there has been any gender-affirming surgery such as a neovagina created in a transgender-affirming or a hysterectomy in a transgender man. Screening and diagnostic tests should be appropriate to the patient’s anatomy that is present, regardless of gender presentation. Patient education regarding screening tests is important. Transgender men who have a cervix may either not understand the need for cervical cancer screening or may avoid screening because of previous trauma or anxiety related to the pelvic exam.26 The HCP should explain to the patient what will take place during the exam including any tests that will be performed beforehand with encouragement to ask questions and/or express any concerns. The patient should be informed that there is the option to decline or defer any part of the exam and that the exam will stop at any time if they request. The HCP can use general terminology for body parts or ask the patient if they have a term or terms they prefer to use. Strategies that may enhance patient comfort include having a support person in the room, using mindfulness techniques, listening to music on headphones or phone, or using other strategies as a distraction during the exam. Patients who desire to be more involved can be offered the use of a mirror to directly observe the exam. Allowing for self-collection of any needed vaginal specimens (eg, wet prep, STI tests) may negate the need for a speculum exam in certain scenarios.26
Principle 3. Adapt practice policies and procedures to maximize inclusion of trans-gender and gender-diverse individuals while minimizing re-traumatization
To determine and evaluate whether or not services are inclusive and respectful, HCPs and staff must engage in constant self-assessment while also requesting feedback from their patients. Intentional efforts to hire and maintain staff, particularly members of the LGBTQ community, that represent diversity in multiple aspects such as gender identity and sexual orientation demonstrate a commitment to inclusivity. Training for new and existing staff is important to develop competency in trauma-informed services for TGNC individuals. It is essential for staff to demonstrate proficiency in these areas. Practice policies that incorporate cultural competency in job descriptions and performance evaluations emphasize its importance. Providing patient brochures on sexually transmitted infection prevention, substance abuse, safe sex practices, mental health, and gender-affirming hormone therapy as well as providing waiting room magazines about the LGBTQ community is equally important.20–24
It should be expected that staff may encounter challenges and part of building a TIC space is to normalize their reactions. Ideally, an open environment for staff is created in which they can discuss their challenges in working with specific populations, explore their own biases, and receive appropriate supervision and training to overcome obstacles.20–24 It is unrealistic to expect that HCPs and staff and patients will completely abandon racist, homophobic, or transphobic thinking. However, it is compulsory to set the expectation for respectful behavior regardless of personal attitudes or experiences.15–19 Working with traumatized and marginalized communities can create vicarious trauma for providers and staff. People who have their own traumatic histories may be triggered by the experiences of patients. Organizational policies can be created and implemented that support staff to recognize their own risks and develop healthy coping strategies.
Conclusion
Effectively implementing a TIC approach to care within a practice takes planning, training, and ongoing evaluation. Exposure to trauma related to gender identity impacts if and how an individual may enter the system of care and respond to it. Thoughtful planning can maximize treatment outcomes and provide a safe, supportive and affirming environment for TGNC individuals seeking care. Ensuring that HCPs and staff have comprehensive training is crucial for creating a healthy care environment. Agency policies and procedures may need to be adapted to promote competent care for TGNC patients and others who have experienced trauma. Including patients who have experienced trauma on advisory committees and agency boards can provide valuable input to ensure culturally competent and accessible care. Effective implementation of a trauma-informed approach to care supports treating all patients in a holistic manner. Trauma-informed practices do their best to ensure that patients do not experience re-traumatization while seeking services.
Research in the area of healthcare for TGNC individuals has increased substantially across multiple disciplines over the last few decades, yet gaps in knowledge remain. More studies are needed to understand the unique trauma experienced by TGNC individuals and to develop best practices to improve care. Curriculum in HCP educational programs and continuing education activities must address TGNC health and healthcare needs. As society becomes more accepting of TGNC individuals, there will be growing opportunities for HCPs, particularly women’s and gender-related health nurse practitioners, to expand care to include gender-affirming therapies in clinical practice. Through research, education, and practice, an underserved and vulnerable population can move out of the shadows and receive care with respect and compassion.
Heather C. Quaile is CEO, Founder, and Clinical Director of the Sexual Health Optimization and Wellness (SHOW) Center in Kennesaw, Georgia. The author has no actual or potential conflicts of interest in relation to the contents of this article.
References
- Reisner SL, Bradford J, Hopwood R, et al. Comprehensive transgender healthcare: the gender affirming clinical and public health model of Fenway Health. J Urban Health. 2015;92(3):584-592.
- Substance Abuse and Mental Health Services Administration. TIP 57: Trauma-Informed Care in Behavioral Health Services. Rockville, MD: SAMHSA; 2014.
- Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. SAMHSA’s Trauma and Justice Strategic Initiative. Rockville, MD: SAMHSA; 2014.
- Quaile HC. Trauma-informed care for the primary care provider. Women’s Healthcare. 2020;8(4):6-12.
- Quaile HC, Benyounes-Ulrich J. Trauma-informed care. Part 1: The road to its operationalization. Women’s Healthcare. 2021;9(3):32-36.
- James SE, Herman JL, Rankin S, et al. The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality; 2016.
- Menschner C, Maul A. Center for Health Care Strategies. Key Ingredients for Successful Trauma-Informed Care Implementation. April 2016.
- Menschner C, Maul A. Center for Health Care Strategies. Strategies for Encouraging Staff Wellness in Trauma-Informed Organizations. December 2016.
- Zaliznyak M, Bresee C, Garcia, MM. Age at first experience of gender dysphoria among transgender adults seeking gender-affirming surgery. JAMA Netw Open. 2020;3(3):e201236.
- Purkey E, Patel R, Phillips SP. Trauma-informed care: better care for everyone. Can Fam Physician. 2018;64(3):170-172.
- Ard KL, Keuroghlian AS. Training in sexual and gender minority health-expanding education to reach all clinicians. N Engl J Med. 2018;379(25):2388-2391.
- Morenz AM, Goldhammer H, Lambert CA, et al. A blueprint for planning and implementing a transgender health program. Ann Fam Med. 2020;18(1):73-79.
- Klein DA, Paradise SL, Goodwin ET. Caring for transgender and gender-diverse persons: what clinicians should know. Am Fam Physician. 2018;98(11):645-653.
- Shires DA, Stroumsa D, Jaffee KD, Woodford MR. Primary care clinicians’ willingness to care for transgender patients, Ann Fam Med. 2018;16(6):555-558.
- Reisner SL, RadixA, Deutsch MB. Integrated and gender-affirming transgender clinical care and research. J Acquir Immune Defic Syndr. 2016;72 suppl 3:S235-S242.
- Bradford J, Reisner SL, Honnold JA, Xavier J. Experiences of transgender-related discrimination and implications for health: Results from the Virginia Transgender Health Initiative Study. Am J Public Health. 2013;103(10):1820-1829.
- Safer JD, Coleman E, Feldman J, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):168-171.
- Goldhammer H, Maston ED, Kissock LA, et a1. National findings from an LGBT healthcare organizational needs assessment. LGBT Health. 2018;5(8):461-468.
- Goldhammer H, Malina S, Keuroghlian AS. Communicating with patients who have nonbinary gender identities. Ann Fam Med. 2018;16(6):559-562.
- US Department of Health and Human Services. Agency for Healthcare Research and Quality. Trauma-informed care. April 2016.
- Knight C. Trauma informed practice and care: implications for field instruction. Clin Social Work J. 2019;47:79-89.
- Key KH. Foundations of Trauma-Informed Care: An Introductory Primer. Baltimore, MD: LeadingAge Maryland; 2018.
- Kinoglu S, Nelson-Dusek S, Skrypek M. Creating a Trauma-Informed Organization: Literature Review for Volunteers of America. St. Paul, MN: Wilder Research; January 2017.
- Hamberger LK, Barry C, Franco Z. Implementing trauma-informed care in primary medical settings: evidence-based rationale and approaches. J Aggression Maltreatment Trauma. 2019;28(4):425-444.
- Shires DA, Stroumsa D, Jaffee KD, Woodford MR. Primary care clinicians’ willingness to care for transgender patients. Ann Fam Med. 2018;16(6):555-558.
- Wesp L. Transgender patients and the physical examination. June 17, 2016.
KEY WORDS: trauma-informed care, transgender, gender nonconforming, gender dysphoria, patient-centered care, people who have experienced trauma

