By Pamela E. Xandre, DNP, WHNP, FNP; Salma Shabaik, MD; and Anita L. Nelson, MD
Pregnancy and pre-conception care (PCC) are major concerns for reproductive-aged women. Although researchers are beginning to find an association between women’s intendedness of pregnancy and their reproductive health-related behaviors, little is known about this topic with respect to Hispanic women in the United States who speak only Spanish. The authors report findings from interviews with 263 members of this population to ascertain their thoughts regarding reproductive life plans and two other topics of interest—PCC and the danger of oral contraceptive use versus pregnancy.
Key words: reproductive life plan, Hispanic women, intendedness of pregnancy, pre-conception care
The ability to choose whether and when to bear children is a fundamental aspect of reproductive health. Yet for more than a decade, about one-half of all pregnancies in the United States have been unintended.1 This statistic represents an average; the proportion of unintended pregnancies varies substantially by demographic group. For example, when compared with non-Hispanic white women, Hispanic women have higher rates of unintended pregnancy, unintended births, and abortions and lower rates of contraception use.2 Rates of unintended pregnancy are substantially increased among poor and low-income women and decreased among higher-income women.2 Poor women are more likely than other women to have unprotected intercourse, and when they do use contraception, they report markedly higher rates of method failure.3,4
Although the reasons are not fully understood and are likely complex, ethnicity, race, culture, and
socioeconomic status all affect decision making about pregnancy and contraceptive use. These factors, alone or in combination, can facilitate or compromise a woman’s ability to formulate a reproductive life plan (RLP) and to meet her RLP goals. These factors can also affect a woman’s knowledge and decisions about pursuing pre-conception care (PCC).
Background
Between 2000 and 2010, the Hispanic population in this country grew by 43% and now comprises 16% of the total U.S. population.5 Compared with non-Hispanic women, Hispanic women have higher rates of unintended pregnancy and lower rates of contraception use. The growing Hispanic population in the U.S. means that healthcare providers (HCPs) will see more and more Hispanic women in their practices and need to know how to help these women make informed decisions about RLPs, use effective contraception when pregnancy is not desired, and obtain PCC to optimize pregnancy outcomes.
Several studies have sought to provide insight into the factors that influence Hispanic women’s decisions about and effective use of contraception. These factors include knowledge about contraception, level of acculturation, attitudes toward planning a pregnancy and toward unintended pregnancy, and attitudes and biases of their HCPs.1,6-8 However, these studies have not focused on Hispanic women who speak only Spanish, or on factors that might influence their RLPs and related decision making about contraceptive use and PCC.
The State of California provides comprehensive family planning and reproductive health services to low-income residents through Family Planning, Access, Care, and Treatment (Family PACT), a federally funded program. In 2010, Family PACT provided services to 1.8 million women and men.9
A sizable proportion of Family PACT clients are Hispanic women who speak only Spanish because they are recent immigrants to this country. This study was conducted with a sample of Spanish-speaking Hispanic women seen at a Family PACT clinic for contraceptive care to explore various aspects of the participants’ RLPs. This study was the first to use CDC guidelines on RLPs and PCC10 as a basis to explore these practices in female members of this ethnic group.
Purpose of study
With the ultimate goal of optimizing women’s health and knowledge before conceiving, the investigators designed a structured interview to determine whether a convenience sample of reproductive-aged, Spanish-speaking women seeking care in a family planning clinic had formulated RLPs. Definitions used by the American College [now Congress] of Obstetricians and Gynecologists (ACOG)11 and in the CDC guidelines for RLPs and PCC10 provided the basis for the interview questions posed in this study.
- A reproductive life plan is defined as a strategy based on a woman’s values and resources to achieve a set of goals about having children, including whether to get pregnant, when to get pregnant, and how many children to have in her lifetime.10 The RLP includes a strategy for effective contraceptive use and options if pregnancy is not desired at all.
- Core pre-conception care involves assessment of a woman’s undiagnosed, untreated, or poorly controlled health conditions; immunization history; medication use; nutritional concerns; genetic risks; substance use; and occupational or environmental exposures prior to conception.11
The investigators sought to answer three questions: (1) Do these women have RLPs? (2) Do they think that women should plan and prepare for pregnancy? and (3) How do they compare the health risks posed by use of birth control pills versus those posed by pregnancy?
Methods and materials
Approval to conduct this study was obtained from the John F. Wolfe Human Subjects Committee and the Research Committee of the Los Angeles Biomedical Research Institute. A 3- to 5-minute interview tool was developed and piloted with 25 potentially eligible women to determine understandability in Spanish and to correct questions that might be confusing. Questions about personal information and RLPs had single answers, and those about pregnancy planning and preparation were open ended (Box).
Neither the term reproductive life plan nor the abbreviation RLP was used when interviewing study participants. Instead, the investigators asked participants how many children they wanted to have and when they wanted to have them. Provision of answers to these questions was considered evidence that a woman had envisioned some form of an RLP for herself. With regard to the question about risks posed by oral contraceptive (OC) use versus pregnancy, the investigators chose to use the term birth control pill as a proxy not only for OCs but for all hormonal contraceptives because they believed that participants would be most familiar with this term.
Interviews were conducted from January 2013 through November 2013 by one of the authors whose first language is Spanish (PX). Prospective participants were approached in the waiting area of the Women’s Health Care Clinic at Harbor UCLA, which provides all types of birth control products to low-income women for free. Women were eligible for the study if they were non-pregnant, Spanish speaking, at least 18 years of age but premenopausal, and at risk for pregnancy. Exclusion criteria were prior hysterectomy or tubal sterilization and lack of ability to give consent. An explanation of the study—including any risks or benefits, assurances of confidentiality, and an option to withdraw at any time without consequences—was read to prospective participants in Spanish. Because the project was an interview with no personal identifiers and no interventions, the Institutional Review Boards approved a waiver of informed consent signature. If a woman gave verbal consent to participate, she was taken to an adjacent private area for the interview. The interviewer used a standard script to ensure uniformity of interview administration and to enable all the data to be merged.
Demographic information was solicited to characterize the study sample. Questions were read aloud and participants’ answers documented verbatim. Participants who did not mention any medical measures in their answer to the question of whether a woman should plan and prepare herself for pregnancy were asked a follow-up question about anything they thought a woman should do medically to plan and prepare for a pregnancy. Medical measures, as described in the CDC guidelines, entail pre-conception screening for health conditions and practices associated with adverse pregnancy outcomes (e.g., obesity, hypertension, smoking).10 The intent of the guidelines is to identify and modify risks before conception occurs. If a participant did not mention any of these medical measures or others, she was asked, Is there any reason for a woman to see a healthcare provider before getting pregnant?
Three investigators placed the participants’ answers to the question about the content of PCC into one of five categories: social, personal, financial, psychological, or medical. Of note, although social, financial, and psychological planning are parts of PCC, this study was designed, at least in part, to find out whether women would include medical measures as part of PCC. If the participants responded with answers that fell into more than one category, each category was tallied. The three investigators had 100% agreement on all category assignments.
Results
A total of 265 women whose primary spoken language was Spanish were approached to participate in the survey. No woman declined, but 2 were excluded because they were surgically infertile; therefore, data for this study were derived from 263 women.
Mean age of the sample was 34 years (range, 18-50 years). Among 263 participants, 4 (1.5%) were younger than 20, 54 (20.5%) were aged 20-25, 42 (15.9%) were aged 26-30, 48 (18.2%) were aged 31-35, and 115 (43.7%) were older than 35. Mean duration of formal education was 10 years (range, 0-18 years). Parity ranged from 0 to 7 births (mode, 2). The time that each woman took to respond to the question about her age was used as the comparator for the speed with which she answered questions about her RLP. Answers to questions were classified as “rapid” if a woman’s response time was at least as fast as when she answered the question about her age, “delayed” if they were more slowly provided, or “unsure” if a woman was unable to provide an answer.
Reproductive life plan
A total of 239 (91%) of the participants said that they knew how many children they wanted to have in their lifetime; among this group, nearly half wanted at least 3 children. A total of 226 women (85.9%) answered this question rapidly, 35 (13.3%) delayed their answers, and 2 (0.8%) were unsure. The 122 women who said that they wanted more children were asked how soon they wanted to become pregnant. Their responses and the speed/assurance of their responses (rapid, delayed, unsure) appear in Table 1.
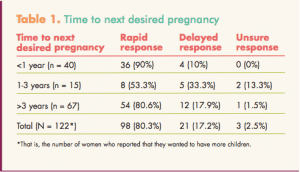
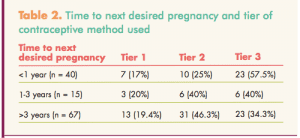
Birth control methods used by these participants were grouped by tiers of efficacy as defined by first-year failure rates in typical use.12Tier I methods include implants, intrauterine devices, and abstinence. Tier 2 methods include pills, patches, vaginal rings, and injections. Tier 3 methods include barrier methods and behavioral methods. Fewer than 20% of women who wanted to delay pregnancy for at least 3 years reported use of tier I methods (Table 2).
Pre-conception care
A total of 252 participants (95.8%) said that a woman should plan and prepare for pregnancy. But when asked how a woman should prepare, only 10.7% provided answers that fell into the category of medical care. More than half of the answers related to financial preparation (26.4%) or mental preparation (26.7%). The remainder of the answers pertained to social preparation (6.3%) or other concerns (13.3%). Even when asked Do you think that there is anything the woman should do to prepare medically for pregnancy? only 2% of the women who had not initially spoken of the need for any medical preparation mentioned PCC at this second opportunity.
Hazards of OC use versus pregnancy
In the last section of the interview, 188 (71.5%) of the participants said that birth control pills were at least as hazardous to a women’s health as pregnancy, whereas only 56 (21.3%) knew that pregnancy was more dangerous than taking birth control pills. Nineteen subjects (7.2%) reported that they did not know which situation was more hazardous.
Discussion
Results of this study suggest that these traditional Hispanic women tended to prize relatively larger families—as compared with the average number of children in U.S. families (~2.4, depending on various definitions of a family by the 2010 Census Bureau).13 Most participants appeared certain about the number of children they wanted and how soon they wanted their next pregnancy. Nevertheless, fewer than one-fifth of those who wanted to delay their next pregnancy for 3 or more years were using a Tier 1 contraceptive method. About one-third were using the least effective Tier 3 methods.
Hispanic women, relative to their non-Hispanic counterparts, know less about reproduction and contraception use, which may partly account for their significantly lower rates of contraceptive use.3,4 Although the findings regarding the use of less effective contraceptive methods by Hispanic women are consistent with other existing research, the purported causes demonstrate that pregnancy planning and contraceptive decision making go beyond simple knowledge. A recent study conducted in Texas, another state with a large Hispanic population, related Hispanic women’s use of less effective contraceptive methods or inconsistent use of methods to their ambivalence about pregnancy.6 In this study, as many as one-third of participants who claimed they wanted no more children still said they would feel very happy or somewhat happy about becoming pregnant in the next 3 months.6 Another study on contraceptive use among young Hispanic women conducted in southeast Texas showed that women low in acculturation (defined by the language portion of the Short Acculturation Scale for Hispanics), compared with women high in acculturation, were more likely to use no contraception or cyclic contraception rather than Tier 1 methods.7 A study by the National Latina Institute for Reproductive Health showed that a large majority of Hispanic women do not use contraception consistently because of economic barriers and deeply rooted cultural and religious influences.2
When asked whether a woman should plan and prepare herself for pregnancy, nearly 96% of the participants responded in the affirmative. However, when asked how a woman should do so, fewer than 11% mentioned anything related to medical aspects of planning and preparation even when prompted. More than 89% gave answers related to psychological, financial, or social planning and preparation. Monitoring a woman’s pre-conception health was not mentioned. Based on these women’s responses, this study population seemed relatively unfamiliar with the importance of medical care prior to becoming pregnant to identify, intervene with, and monitor pre-conception risk to improve pregnancy outcomes. No other studies looking specifically at Hispanic women’s knowledge or attitudes related to PCC were found.
When asked whether they thought birth control pills or pregnancy was more hazardous to a woman’s health, more than 70% of participants chose the former—even though pregnancy is far more dangerous than use of any of the hormonal contraceptives.14 These women, like most U.S. women, believe that pregnancy is a natural process that could not possibly be riskier to their health than hormonal contraceptive use. In fact, a study of English-speaking, reproductive-aged women’s knowledge of the health risks of pregnancy versus those risk of OC use showed the same misconceptions.14 Even the more highly educated, affluent women in this study considered OC use more hazardous than pregnancy.
Study limitations
Generalizability of these study findings is limited. The data were derived from an interview of Hispanic women, many of whom were recent immigrants to the U.S., at a single clinic for low-income women. The results do not represent women in general or Spanish-speaking Hispanic women. Another concern is that more than half (53.6%) of these participants had completed their families and wanted no more pregnancies. However, this subgroup provided the investigators with important insights into the mismatch between their pregnancy plans and their selection of less effective contraceptive methods.
Practice implications
This survey revealed three important points. First, HCPs need to be aware that many Spanish-speaking women may not have clearly defined their fertility goals. Rather than asking a woman whether she plans to get pregnant in the next year, HCPs should ask, How would you feel if you were to get pregnant in the next year? Her answer may reveal her commitment or ambivalence regarding pregnancy prevention, which is important to know when prescribing a user-dependent birth control method. For women seeking contraception who are ambivalent about pregnancy prevention, HCPs may want to plan for follow-up to address any concerns that might arise during early use of the method.15
Second, HCPs need to directly address women’s concerns about contraceptive safety.7,12 HCPs should assess each woman’s contraceptive experiences and preferences. This assessment may help uncover misconceptions, fears, or the influences of others on her contraceptive decision making.15 Use of less effective contraceptive methods (i.e., those in Tier 3) may reflect her concerns about the safety of using more effective methods (i.e., those in Tiers 1 and 2). Every time HCPs prescribe a particular method, a patient should be informed that this method is safer for her than pregnancy.
Third, to address a Spanish-speaking, reproductive-aged woman’s lack of familiarity with the importance of PCC, HCPs should routinely remind her that, if and when she wants to get pregnant, she should return to have her health status evaluated and to learn what she can do to improve the outcome of the intended pregnancy. Every family planning visit provides an opportunity for pre-conception counseling on healthy lifestyle behaviors and pre-pregnancy management of risk factors and medical conditions that influence pregnancy outcomes.
Conclusion
Lack of pregnancy planning and inconsistency between stated pregnancy plans and effective contraceptive use are common among U.S. women.16 The findings of this study reflect the need to continue to expand HCPs’ understanding of the causes for this inconsistency in both the general population and in specific populations.
Pamela E. Xandre is Assistant Professor at the School of Nursing, California State University, Long Beach. Salma Shabaik is a physician at Family Practice in Long Beach, California. Anita L. Nelson is Professor in the Department of Obstetrics and Gynecology at the David Geffen School of Medicine, University of California at Los Angeles. The authors state that they do not have a financial interest in or other relationship with any commercial product named in this article.
References
1. Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006; 38(2):90-96.
2. Ranjit N, Bankole A, Darroch JE, Singh S. Contraceptive failure in the first two years of use: differences across socioeconomic subgroups. Fam Plann Perspect. 2001;33(1):19-27.
3. Sangi-Haghpeykar H, Ali N, Posner S, Poindexter AN. Disparities in contraceptive knowledge, attitudes, and use in Hispanic and non-Hispanic whites. Contraception. 2006;74(2): 125-132.
4. Schwarz EB, Smith R, Steinauer J, et al. Measuring the effects of unintended pregnancy on women’s quality of life. Contraception. 2008;78(3): 204-210.
5. Humes KR, Jones NA, Ramirez RR. Overview of race and Hispanic origin, 2010. Census Briefs. March 2011. census.gov/prod/cen2010/briefs/c2010br-02.pdf
6. Aiken AR, Potter JE. Are Latina women ambivalent about pregnancies they are trying to prevent? Evidence from the Border Contraceptive Access Study. Perspect Sex Reprod Health. 2013;45(4):196-203.
7. Roncancio AM, Ward KK, Berenson AB. The use of effective contraception among young Hispanic women: the role of acculturation. J Pediatr Adolesc Gynecol. 2012;25(1):35-38.
8. Rocca CH, Harper CH. Do racial and ethnic differences in contraceptive attitudes and knowledge explain disparities in method use. Perspect Sex Reprod Health. 2012;44(3):150-158.
9. California Department of Healthcare Services. Fact Sheet on Family PACT: An Overview. Updated January 2012. familypact.org/Providers/Fact-sheets/2-2012_FamPACT_FS_Overview_2-15ADA.pdf
10. Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care—United States: a report of the CDC/ATSDR Preconception Work Group and the Select Panel on Preconception Care. Morbid Mortal Weekly Rep. 2006;55(RR-06):1-23.
11. American College of Obstetricians and Gynecologists. ACOG Committee Opinion number 313, September 2005. The importance of pre-conception care in the continuum of women’s health care. Obstet Gynecol. 2005;106(3):665-666.
12. Wysocki S. The state of hormonal contraception today: enhancing clinician/patient communications. Am J Obstet Gynecol. 2011;205(4 suppl):S18-S20.
13. United States Census Bureau. America’s Families and Living Arrangements: 2010. census.gov/
population/www/socdemo/hh-fam/cps2010.html
14. Nelson AL, Rezvan A. A pilot study of women’s knowledge of pregnancy health risks: implications for contraception. Contraception. 2012;85(1):78-82.
15. Gavin L, Moskosky S, Carter M, et al; Centers for Disease Control and Prevention. Providing quality family planning services: recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep. 2014;63(RR-04):1-54.
16. Morgan SP, Rackin H. The correspondence between fertility intentions and behavior in the United States. Popul Dev Rev. 2010;36(1):91-118.

