Infertility affects approximately 11% of women and 9% of men in the United States who are of reproductive age.1 Patients diagnosed with infertility report high levels of distress, most commonly generalized anxiety disorder closely followed by major depressive disorder.2 Approximately 40% of women being evaluated prior to their first infertility consult screened positive for depression and anxiety, twice as many as the general population.3,4 Infertility patients experiencing depression and anxiety may report a reduction in quality of life, including problems with relationships, intimacy, and even spirituality.2 Infertility has also been shown to affect careers and personal finances.2 Most infertility patients and partners are neither being provided information on mental health services nor being given mental health provider referrals.5 These data suggest that depression and anxiety in infertility patients are significant issues and need to be addressed. The US Preventive Services Task Force (USPSTF) recommends that screening for depression be offered for adults in the general population, while making readily available protocols to adequately diagnose, refer, treat, and manage appropriately.6 Screening for depression has been given a B grade per the USPSTF.6 Practices should offer this service, as the overall benefit is moderately substantial.6 Healthy People 2030 mental health and mental disorders objective 08 states that the target goal for depression screening for adolescents and adults should increase from 8.5% to at least 13.5%.7 Although both the USPSTF and Healthy People 2030 focus on screening for depression only, anxiety is known to accompany depression, and typically depression follows untreated anxiety.3
Project purpose
The purpose of this project was to implement a depression and anxiety screening tool and management protocol to improve risk assessment, management and potential treatment of depression and anxiety in infertility patients. The aim of the quality improvement (QI) project was to improve depression and anxiety screening in an infertility practice from 0% to 75% through education and integration of a screening tool and a treatment algorithm.
Description of population and setting
This project was implemented in two clinics of a multisite reproductive endocrinology practice for the 5-month pilot study. There were two target groups for this implementation. Physicians, nurse practitioners, physician’s assistants, registered nurses, medical assistants, and front desk personnel staff were one target group. New primary patients seen by one physician 4 days a week comprised the other group. To clarify, a primary patient was defined as the patient whom the appointment was scheduled under, while their partner, if applicable, was linked to the primary patient’s profile. This project was reviewed by the University of Colorado at Colorado Springs Institutional Review Board confirming this study did not qualify as human subject research.
Description of quality improvement project
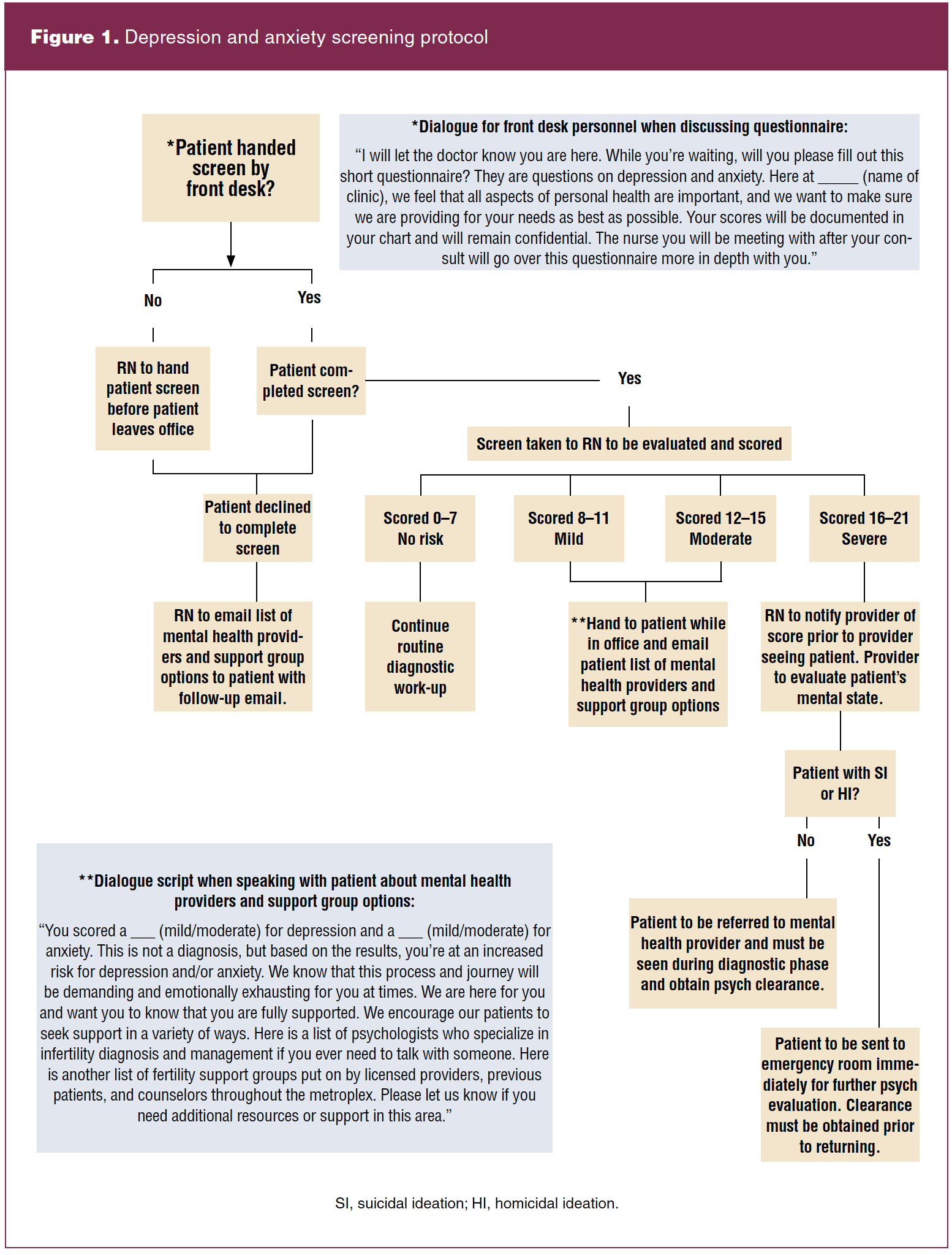
A mental healthcare needs assessment was completed by the project director. This included the knowledge of the staff regarding depression and anxiety in the clinic’s patient population, the screening processes utilized, and available mental health resources within the practice. This information was presented to all staff including a physician, nurses, medical assistants, and front desk personnel prior to the start of the pilot study to establish a baseline. The needs assessment was followed by an initial lunch and learn, incorporating a pre- and post-discussion quiz highlighting depression and anxiety in infertility, and detailing the new proposed screening process. Instruments utilized included the workflow algorithm created by the project director with help from the office staff as seen in Figure 1 and the Hospital Anxiety and Depression Scale (HADS). The HADS screen identifies those at risk for developing depression and anxiety, consists of 14 questions, and is easy to complete and score.8 The HADS screen has been validated in infertility practice patients.8
The algorithm detailed the new process for provision of the screen to the primary patient by the front desk staff, scored by the nurse, documented in the patient’s chart, and followed up with the appropriate action by the nurse based on the patient’s score (Figure 1). Scoring for the HADS scale is as follows: equal to or less than 7 is scored as a non-case, 8 to 10 as mild, 11 to 14 as moderate, and 15 to 21 as severe. It was decided as a practice that all patients scoring in the mild, moderate, or severe range would be provided with support group options and mental health provider referral information. For those who scored in the severe range, documentation and immediate follow-up with a mental health provider would be required prior to moving forward with fertility treatment.
Methods to evaluate outcome
Staff pre- and post-quiz scores were evaluated to determine understanding of the content presented.
Patient identification numbers and their HADS score were collected monthly via manual chart reviews and logged into an Excel spread sheet accessible by the project director. In both locations, screening rates were determined by comparing numbers of new patients screened with total numbers of new patient encounters.
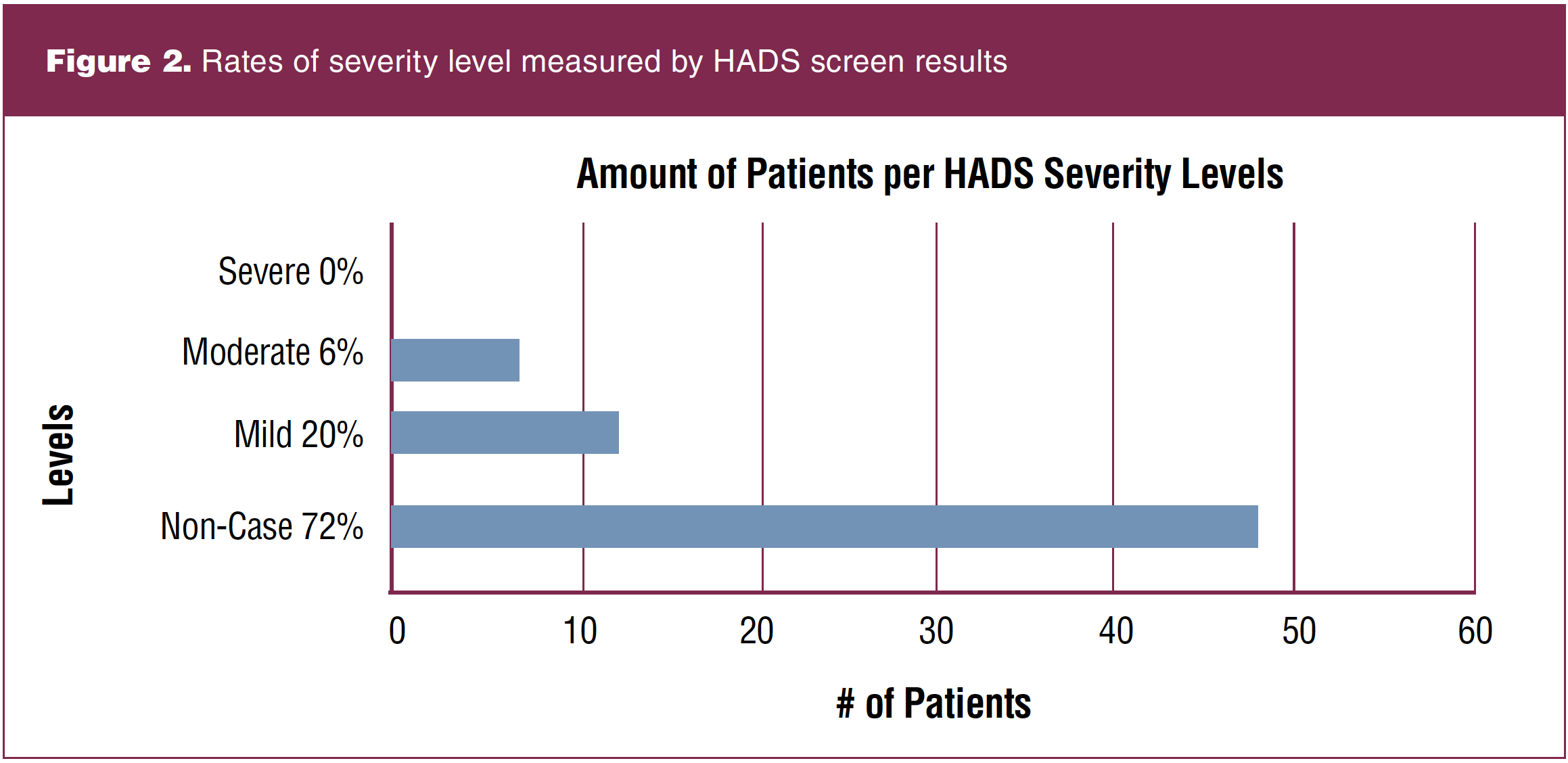
An analysis of the HADS score determined the level of depression and anxiety, providing guidance for resource and referral needs.
Outcomes
There were 98 new fertility patients, all female, seen by the physician at both practice locations from July 27, 2020, through December 31, 2020. Sixty-seven were correctly handed the screen for depression and anxiety, while 31 patients were not. Two patients declined to fill out the form altogether. Screening new patients for depression and anxiety increased from 0% prior to the interventions to 68% at the end of the 5 months. Mental health resources were provided to 100% of the patients who scored in the mild, moderate, or severe categories on the HADS screen (Figure 2).
Eight staff members participated in staff education, and 4 of the 8 (50%) improved their score between the pre- and post-lunch and learn quizzes that included four questions each. After the lunch and learn, all eight (100%) participants reported that they felt better prepared to use the HADS screen and new algorithm, and the education was effective in understanding depression and anxiety within the infertility population.
Discussion and implications for practice
Greater than one fourth of all providers admit to not screening their patients due to lack of knowledge regarding treatment recommendations and time available.9 We implemented a depression and anxiety screening tool and algorithm that resulted in the screening rate increasing from 0% to 68% in response to the evidence that psychological disorders negatively affect fertility treatment and pregnancy outcomes.9 Given depression and anxiety rates and the increase in numbers of women seeking infertility treatment, capturing this population allows for early detection, treatment, and management of depression and anxiety, which has implications for overall health and wellbeing.
Within the fertility practice, “satellite champions” were identified following the conclusion of the pilot study for the three other locations. In meeting with the champions, the algorithm screening process was explained, allowing room for questions and adjustments based on the individual office. As the screening process is implemented across the entire company, the satellite champions will continue to monitor and manage screening patients, thus allowing for longevity and sustainability.
Process improvement cycles were helpful when implementing the screening process. For example, staff needed briefing or reeducating to be sure that the front desk personnel remembered to provide new patients with the screening tool. To mitigate this issue, copies of the screen were made and placed into the patient folders that were prepared for the following day each afternoon. Another example of process improvement was reeducation surrounding the mis-scoring of the HADS tool. Individual and group teachings were completed throughout the pilot timeframe to confirm continual understanding of the scoring and process.
Conclusion
Limitations
The private practice consists of five locations. Rotation of nurses and front desk personnel due to paid time off coverage affected outcomes, as the new process was not consistently communicated to the temporary staff. The current pandemic required a pivot to telehealth, and screening was not conducted for telehealth appointments. Implementing this QI project into a busier practice could potentially increase the length of time it takes to hand out, return and score the screen, educate the patient on resources, and document the process. When implementing the new process in the other practice sites, it would be helpful to quantify time needed for the implementation process, something that was not done in this project. Another limitation of note was the omission of a plan for screening same-sex couples, or the male partner of a heterosexual couple. Future implementation should address processes for screening both the primary patient and the significant other.
In conclusion, the successful implementation of a depression and anxiety screening process into an infertility practice demonstrates feasibility for the other offices of the practice and meets important recommendations for addressing mental health needs during the infertility journey. Having the ability to recognize those at an increased risk for depression and anxiety early on in their fertility journey can positively affect the patient’s wellbeing as well as the probability of impacting their fertility treatment outcomes.
Kimberly L. Walker is currently practicing at Alpine Women’s Centre in Montrose, Colorado. Judith M. Scott is Assistant Professor and coordinator for the RN to BSN program at Helen & Arthur E. Johnson Beth-El College of Nursing and Health Sciences at the University of Colorado, Colorado Springs. The authors have no actual or potential conflicts of interest in relation to the contents of this article.
References
1 US Department of Health and Human Services, National Institute of Health. How common is infertility? 2018. https://www.nichd.nih.gov/health/topics/infertility/conditioninfo/common.
2 Domar AD. Creating a collaborative model of mental health counseling for the future. Fertil Steril. 2015;104(2):277-280.
3 National Institute of Mental Health. Anxiety disorders. 2017. https://www.nimh.nih.gov/health/topics/anxiety-disorders/index.shtml.
4 Crawford NM, Hoff HS, Mersereau JE. Infertile women who screen positive for depression are less likely to initiate fertility treatments. Hum Reprod. 2017;32(3):582-587.
5 Pasch LA, Holley SR, Bleil ME, et al. Addressing the needs of fertility treatment patients and their partners: are they informed of and do they receive mental health services? Fertil Steril. 2016;106(1):209-215.
6 Siu AL, et al; US Preventive Services Task Force. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(4):380-387.
7 Office of Disease Prevention and Health Promotion. Healthy People 2030. Social determinants of health. https://health.gov/healthypeople/objectives-and-data/social-determinants-health.
8 Massarotti C, Gentile G, Ferreccio C, et al. Impact of infertility and infertility treatments on quality of life and levels of anxiety and depression in women undergoing in vitro fertilization. Gynecol Endocrinol. 2019;35(6):485-489.
9 Hoff Hs, Crawford NM, Mersereau JE. Screening for psychological conditions in infertile women: provider perspectives.
J Womens Health. 2018;27(4):503-509.